Focus on consistent, moderate exercise. Start with gentle activities like walking for 20-30 minutes daily, gradually increasing duration and intensity as tolerated. Physical therapy, specifically tailored to address muscle weakness, significantly accelerates recovery. Your therapist will guide you through exercises improving strength and range of motion.
Nutrition plays a crucial role. Prioritize a balanced diet rich in protein to support muscle repair. Lean meats, fish, beans, and lentils are excellent choices. Include plenty of fruits and vegetables for essential vitamins and minerals. Consult a registered dietitian for personalized dietary advice, considering your specific needs and any other health conditions.
Monitor your progress closely. Regular check-ups with your doctor are vital for tracking muscle strength recovery and adjusting treatment plans as needed. Be patient; recovery takes time, and individual experiences vary. Open communication with your healthcare team ensures you receive the support and guidance needed throughout your recovery.
Consider supplements. After consulting your doctor, you might benefit from creatine or other supplements to aid muscle growth and repair. However, remember that these are only supportive, not replacement, for proper diet and exercise. Always adhere to recommended dosages.
- Prednisone Myopathy Recovery: A Comprehensive Guide
- Nutrition and Hydration for Recovery
- Managing Pain and Inflammation
- Monitoring Progress and Seeking Support
- Lifestyle Adjustments for Long-Term Well-being
- Addressing Specific Muscle Groups
- Understanding Potential Setbacks
- Understanding Prednisone-Induced Myopathy
- Recognizing the Symptoms of Prednisone Myopathy
- Muscle Pain and Tenderness
- Fatigue and Reduced Physical Endurance
- Difficulty with Physical Activities
- Muscle Atrophy (Muscle Wasting)
- Other Potential Symptoms
- The Role of Physical Therapy in Recovery
- Dietary Adjustments to Support Muscle Recovery
- Prioritizing Micronutrients
- Addressing Potential Complications
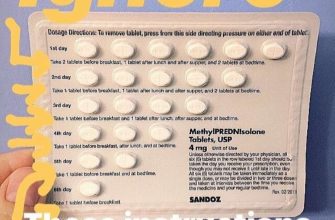
- Medication Management and Tapering Prednisone
- Understanding the Tapering Process
- Managing Potential Side Effects
- Monitoring Your Progress
- Alternative Medications
- Monitoring Progress and Potential Complications
- When to Seek Medical Attention During Recovery
- Monitor Your Progress Closely
- Understanding Your Recovery Timeline
- When to Consider Additional Support
- Signs Requiring Immediate Medical Attention
- Your Doctor’s Role in Recovery
Prednisone Myopathy Recovery: A Comprehensive Guide
Begin physical therapy immediately after your Prednisone course ends, focusing on exercises tailored to your specific muscle weaknesses. A physical therapist will design a program promoting strength and flexibility. Consistent engagement is key.
Nutrition and Hydration for Recovery
Prioritize a balanced diet rich in protein to support muscle repair. Lean meats, fish, beans, and lentils are excellent choices. Stay well-hydrated; water aids muscle function and overall recovery.
Managing Pain and Inflammation
Your doctor might prescribe medications to manage pain and inflammation, such as NSAIDs or other anti-inflammatory drugs. Discuss potential side effects and follow prescribed dosages carefully. Gentle stretches can also ease muscle stiffness.
Monitoring Progress and Seeking Support
Regular check-ups with your doctor are critical to track your progress. Openly discuss any concerns or setbacks. Support groups can provide valuable emotional and practical advice from others undergoing similar experiences. Remember, recovery takes time and patience; celebrate small victories along the way.
Lifestyle Adjustments for Long-Term Well-being
Moderate exercise, even after full recovery, maintains muscle strength and overall health. Avoid strenuous activity during the recovery phase. Prioritizing sleep and stress management promotes faster healing and prevents future muscle problems.
Addressing Specific Muscle Groups
Proximal muscle weakness, common in Prednisone myopathy, requires targeted exercises for the shoulders, hips, and thighs. Your physical therapist will identify areas needing extra attention and create exercises specifically for these areas. Consistency and proper form are vital to prevent further injury.
Understanding Potential Setbacks
Some individuals experience a slower recovery than others. Don’t get discouraged by occasional setbacks. Report any worsening symptoms to your doctor, who can adjust treatment plans accordingly. Persistence is crucial for optimal outcomes.
Understanding Prednisone-Induced Myopathy
Prednisone, while effective for many conditions, can cause muscle weakness and wasting – a condition known as prednisone-induced myopathy. This often manifests as proximal muscle weakness, meaning weakness in the muscles closest to your body’s core, like your shoulders and hips.
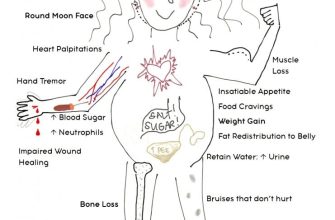
Several factors influence the severity: dosage, duration of treatment, and individual susceptibility. Higher doses and longer treatment periods increase the risk.
- High-dose prednisone (over 7.5mg daily for extended periods) significantly raises your risk.
- Concurrent conditions such as diabetes, osteoporosis, and hypothyroidism can exacerbate muscle problems.
- Age plays a role; older adults are more vulnerable.
Recognizing symptoms is key to early intervention. These can include:
- Difficulty climbing stairs or rising from a chair
- Muscle pain and tenderness
- General fatigue and weakness
- Decreased muscle mass
Your doctor may order blood tests to assess muscle enzyme levels (CK) which often elevate in myopathy. A physical examination will assess your muscle strength. In some cases, additional imaging like MRI might be used.
Recovery depends on several factors. The most important step is addressing the underlying cause. Your doctor may gradually reduce your prednisone dosage, possibly switching to alternative treatments where appropriate. A tailored exercise program, focusing on low-impact activities to rebuild muscle strength, is crucial. A dietitian can also provide guidance on nutrition to promote muscle recovery.
- Gradual Prednisone Tapering: Your doctor will carefully reduce your prednisone dose to minimize withdrawal symptoms and muscle recovery problems.
- Physical Therapy: A regimen of targeted exercises, tailored to your needs, helps restore strength and function.
- Nutritional Support: A balanced diet rich in protein and other essential nutrients is essential for muscle repair.
- Regular Monitoring: Consistent checkups with your doctor are important to track progress and adjust treatment as needed.
While recovery time varies, consistent adherence to your doctor’s recommendations significantly improves your chances of regaining muscle strength and function.
Recognizing the Symptoms of Prednisone Myopathy
Pay close attention to changes in your muscle strength and function. Weakness, particularly in your proximal muscles (those closest to your body’s core, like your shoulders and hips), is a key indicator. You might find it harder to climb stairs, rise from a chair, or lift objects. This weakness can develop gradually.
Muscle Pain and Tenderness
Muscle aches and tenderness are common. The pain might be diffuse or localized, and worsen with activity. Rest might offer some relief, but the pain can persist even at rest. Note the location and intensity of the pain to help your doctor.
Fatigue and Reduced Physical Endurance
Prednisone-induced muscle weakness often leads to significant fatigue. Simple tasks can become exhausting. This fatigue goes beyond typical tiredness; it’s a profound lack of energy impacting your daily life. Monitor your energy levels to track progression.
Difficulty with Physical Activities
Observe how your physical capabilities change. Difficulty performing everyday activities, such as brushing your hair, reaching overhead, or walking longer distances, are significant signs. These functional limitations directly result from the muscle weakness.
Muscle Atrophy (Muscle Wasting)
In more severe cases, you may notice a reduction in muscle bulk. This muscle wasting is visible as a decrease in muscle size and can affect various muscle groups. This is a late-stage manifestation, requiring prompt medical attention.
Other Potential Symptoms
Important: While the above are primary symptoms, you may also experience other issues like increased bone fragility, leading to fractures, or an altered gait. Report any unexpected symptoms to your doctor immediately.
The Role of Physical Therapy in Recovery
Begin with low-impact exercises like walking to gradually rebuild strength and endurance. Your physical therapist will create a personalized program tailored to your specific needs and limitations.
Expect regular sessions focusing on range-of-motion exercises to improve flexibility and prevent joint stiffness. These exercises should address any muscle weakness or atrophy caused by Prednisone.
Strengthening exercises, such as resistance training with light weights or resistance bands, are key to regaining muscle mass and function. Your therapist will guide you on proper form to prevent injury.
Balance and coordination exercises are also important, particularly as Prednisone can affect your sense of equilibrium. These help prevent falls and improve overall stability.
Active participation is crucial. Follow your therapist’s instructions carefully and perform home exercises diligently. Consistency is vital for optimal recovery.
Regular check-ins with your physical therapist allow them to monitor your progress, adjust your program as needed, and address any concerns that arise during your recovery.
Expect a gradual improvement. Recovery time varies, depending on factors such as the severity of your myopathy and your individual response to therapy. Be patient and celebrate small victories along the way.
Dietary Adjustments to Support Muscle Recovery
Prioritize protein intake. Aim for 1.2-1.6 grams of protein per kilogram of body weight daily. Lean protein sources like chicken breast, fish, and beans are excellent choices. This supports muscle protein synthesis, crucial for rebuilding muscle tissue.
Prioritizing Micronutrients
Consume foods rich in vitamin D. Vitamin D deficiency is common and can worsen muscle weakness. Increase your intake through sunlight exposure (safely!) or supplements, as advised by your doctor. Furthermore, ensure adequate intake of vitamin B12 and potassium, which play vital roles in muscle function. Consider foods like eggs, fortified cereals, and leafy greens.
Increase your intake of healthy fats. Omega-3 fatty acids, found in fatty fish like salmon and tuna, have anti-inflammatory properties that can help reduce muscle pain and inflammation. Incorporate them into your diet regularly.
Stay hydrated. Dehydration can exacerbate muscle weakness. Drink plenty of water throughout the day. Monitor your urine color; pale yellow is ideal. Electrolyte drinks might be helpful during periods of intense exercise, but consult your doctor.
Addressing Potential Complications
Avoid excessive sugar and processed foods. These contribute to inflammation and can hinder muscle recovery. Opt for whole, unprocessed foods whenever possible.
Consult a registered dietitian or nutritionist. They can personalize a dietary plan based on your individual needs and medical history, ensuring you receive the right nutrients for optimal recovery.
Medication Management and Tapering Prednisone
Always follow your doctor’s instructions precisely for Prednisone dosage and tapering schedule. This is paramount for minimizing muscle weakness and promoting recovery.
Understanding the Tapering Process
Prednisone withdrawal must be gradual. Sudden stops can trigger serious side effects. Your doctor will create a personalized tapering plan, usually involving a slow reduction in dosage over weeks or months. This plan considers your individual health, Prednisone dosage, and response to treatment.
- Expect regular blood tests to monitor your progress and adjust the tapering schedule as needed.
- Be prepared for potential side effects during the tapering phase. These may include fatigue, joint pain, and muscle weakness (although usually less severe than during initial Prednisone use).
- Report any concerning symptoms to your physician immediately. Don’t hesitate to contact them if you experience increased muscle weakness, severe pain, or other troubling changes.
Managing Potential Side Effects
Communicate openly with your physician regarding any side effects. They can offer strategies to manage them, such as:
- Prescribing medications to address specific side effects (e.g., pain relievers for joint pain).
- Suggesting physical therapy to improve muscle strength and range of motion.
- Recommending lifestyle adjustments (e.g., increased rest, modified exercise).
Monitoring Your Progress
Active participation in your recovery is vital. Track your symptoms (muscle strength, pain levels, energy levels) and report any changes to your doctor. This aids them in optimizing your tapering plan.
Alternative Medications
In some cases, your doctor may prescribe alternative medications to help manage your condition and minimize the reliance on Prednisone or its associated side effects. Discuss this possibility with your physician.
Monitoring Progress and Potential Complications
Regularly track your muscle strength using a simple strength test, like lifting weights or performing bodyweight exercises. Note any improvement or worsening of symptoms. Document your progress in a journal or app.
Schedule follow-up appointments with your doctor as advised. These visits allow for objective assessment of your muscle function through examinations and potentially blood tests to monitor for muscle damage markers like creatine kinase (CK).
Pay close attention to your weight. Unexplained weight gain could indicate fluid retention, a side effect of prednisone. Conversely, significant weight loss might point to muscle wasting.
Monitor for signs of osteoporosis, such as bone pain or increased fragility. Prednisone can weaken bones, so discuss bone density testing with your physician.
Watch for signs of infection, as prednisone can suppress your immune system. Report any fever, chills, or persistent cough immediately to your doctor.
Report any new or worsening symptoms like severe muscle weakness, significant pain, difficulty swallowing, breathing problems, or changes in vision. These may indicate serious complications requiring prompt medical attention.
Maintain a healthy diet rich in protein and calcium to support muscle repair and bone health. Incorporate regular, gentle exercise into your routine as tolerated, gradually increasing intensity as you feel stronger. Always discuss your exercise plan with your doctor.
Open communication with your healthcare provider is key. Don’t hesitate to discuss any concerns you have throughout your recovery process.
When to Seek Medical Attention During Recovery
Contact your doctor immediately if you experience worsening muscle weakness, especially if it affects your breathing or swallowing. Don’t hesitate to call.
Seek immediate medical attention if you develop new symptoms such as fever, increased pain, or significant swelling in your muscles. These could indicate an infection or other complication.
Monitor Your Progress Closely
Keep a close eye on your strength levels. If your progress plateaus for more than a week, or if you notice a decline, schedule an appointment with your physician.
Understanding Your Recovery Timeline
Recovery times vary. While some individuals see significant improvement within weeks, others may require months. Don’t compare your recovery to others; focus on your own progress. Consistent monitoring is key.
When to Consider Additional Support
Physical therapy can significantly aid your recovery. If you’re struggling to regain strength or mobility, consult your doctor about a referral.
Signs Requiring Immediate Medical Attention
| Symptom | Action |
|---|---|
| Severe muscle weakness affecting breathing or swallowing | Go to the emergency room immediately |
| Sudden onset of fever or chills | Contact your doctor immediately |
| Increased muscle pain or swelling | Contact your doctor immediately |
| Persistent muscle weakness despite therapy | Schedule an appointment with your doctor |
Your Doctor’s Role in Recovery
Your physician can provide guidance, monitor your progress, and adjust your treatment plan as needed. Open communication is crucial for optimal recovery.