Prednisone can significantly reduce inflammation and pain during rheumatoid arthritis (RA) flares. Doctors often prescribe it for short-term, high-dose treatment to quickly control symptoms. Remember, it’s not a long-term solution; tapering off the medication under medical supervision is crucial.
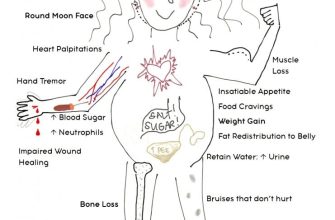
Typical dosages range from 20 to 60 mg daily, depending on the severity of your flare. Your rheumatologist will determine the appropriate dose and duration. Closely monitor side effects; common ones include weight gain, increased blood sugar, and mood changes. Report any concerning symptoms immediately.
While Prednisone provides rapid relief, it’s important to address the underlying RA. Combine Prednisone with your regular disease-modifying antirheumatic drugs (DMARDs) to achieve long-term control. Maintaining a healthy lifestyle–including regular exercise and a balanced diet–also plays a key role in managing RA.
Consult your doctor before starting or stopping any medication, including Prednisone. They can help you develop a personalized treatment plan to manage your RA flares and minimize potential side effects. Understanding the proper use of Prednisone empowers you to actively participate in your healthcare.
- Prednisone for Rheumatoid Arthritis Flares: A Quick Guide
- Understanding Prednisone’s Role in RA Flare Management
- Dosage and Administration: What to Expect When Taking Prednisone
- Common Dosages and Administration
- What to Expect
- Important Considerations
- When to Consult Your Doctor: Recognizing Potential Complications
- Monitoring for Side Effects
- Medication Interactions
Prednisone for Rheumatoid Arthritis Flares: A Quick Guide
Prednisone rapidly reduces inflammation, offering significant RA flare relief. Expect symptom improvement within days, often feeling better within 24-72 hours.
Dosage varies depending on your individual needs and the severity of your flare. Your doctor will determine the appropriate dose and duration of treatment. Typically, treatment is short-term to minimize side effects.
Common side effects include weight gain, increased appetite, insomnia, mood changes, and increased blood sugar. Discuss any concerns with your rheumatologist.
Tapering off Prednisone is crucial to prevent a relapse and reduce the risk of side effects. Your doctor will create a gradual tapering schedule, slowly decreasing your dosage over several weeks or months. Never stop taking Prednisone abruptly.
Long-term Prednisone use carries increased risks. This medication is for flare management, not ongoing treatment. Your doctor will focus on managing your RA with disease-modifying antirheumatic drugs (DMARDs) for long-term control.
Regular monitoring is necessary during Prednisone treatment. Your doctor will schedule appointments to track your progress, assess side effects, and adjust your medication as needed.
Contact your doctor immediately if you experience severe side effects or your symptoms worsen despite treatment. Open communication with your rheumatologist is key to effective flare management.
Understanding Prednisone’s Role in RA Flare Management
Prednisone quickly reduces inflammation and pain during rheumatoid arthritis flares. This powerful anti-inflammatory steroid works by suppressing your immune system’s activity, lessening the attack on your joints.
Doctors typically prescribe prednisone for short-term use to control a flare, aiming for the lowest effective dose and the shortest duration. This minimizes potential side effects. Your rheumatologist will develop a tapering schedule to gradually reduce your dosage over several weeks to avoid withdrawal symptoms.
Common side effects include weight gain, increased appetite, mood changes, and insomnia. These usually lessen as the dose decreases. Severe side effects are rare but should be reported immediately to your doctor. Regular monitoring of blood pressure and blood sugar might be necessary, particularly for individuals with pre-existing conditions.
Prednisone isn’t a long-term solution for RA. It manages flares; it doesn’t cure the disease. Your doctor will likely also prescribe disease-modifying antirheumatic drugs (DMARDs) for long-term management to slow disease progression. Combining prednisone with DMARDs offers a comprehensive approach to managing rheumatoid arthritis.
Always discuss any concerns about prednisone or your treatment plan with your doctor or rheumatologist. They can help you weigh the benefits against the risks and create a personalized plan to best manage your RA.
Dosage and Administration: What to Expect When Taking Prednisone
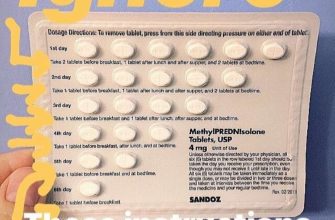
Your doctor will determine the appropriate prednisone dosage based on your individual needs and the severity of your rheumatoid arthritis flare. This is usually a short course, not a long-term solution. Expect your doctor to prescribe a specific daily dose and a clear plan for gradually reducing the dose over time, typically by a small amount every few days. This tapering process minimizes potential side effects.
Common Dosages and Administration
Prednisone is typically taken orally, once daily, usually in the morning with food to reduce stomach upset. Common starting dosages for rheumatoid arthritis flares range from 20mg to 60mg daily, but this varies greatly by patient. The duration of treatment also depends on your response. Always follow your doctor’s instructions precisely; never adjust your dosage without consulting them.
What to Expect
- Improved Symptoms: You should notice a reduction in pain, swelling, and stiffness within a few days to a week. The exact timeline depends on your body’s response.
- Side Effects: While prednisone is effective, it can cause side effects. Common ones include increased appetite, weight gain, mood changes, insomnia, increased blood sugar, and increased risk of infection. These side effects are usually manageable and often lessen as the dosage is reduced.
- Monitoring: Regular blood tests may be needed to monitor your progress and identify any potential side effects. Your doctor will discuss this with you.
- Tapering Schedule: A gradual reduction in dosage is critical to avoid withdrawal symptoms, which can include fatigue, muscle aches, and joint pain. Strictly adhere to the tapering schedule provided by your doctor.
Important Considerations
- Inform Your Doctor: Report any new or worsening symptoms to your doctor immediately. This includes any side effects.
- Medication Interactions: Prednisone can interact with other medications. Be sure your doctor is aware of all medications you are taking, including over-the-counter drugs and supplements.
- Lifestyle Adjustments: Maintaining a healthy diet, exercising regularly, and getting adequate rest can help manage your condition and reduce the impact of prednisone side effects.
Remember, this information is for general knowledge and does not constitute medical advice. Always consult your doctor or rheumatologist for personalized guidance on prednisone use for rheumatoid arthritis flares. They can assess your specific situation and provide the most appropriate treatment plan.
When to Consult Your Doctor: Recognizing Potential Complications
Contact your doctor immediately if you experience any of the following: severe abdominal pain, unexplained weight gain, persistent nausea or vomiting, blurred vision, increased thirst or urination, easy bruising or bleeding, severe muscle weakness, or signs of infection such as fever, chills, or persistent cough.
Monitoring for Side Effects
Regularly monitor your blood pressure and blood sugar levels as directed by your doctor. Report any significant changes. Keep a record of your symptoms and medication doses to share with your physician. Pay close attention to any changes in your mood, such as increased anxiety or depression. These are potential side effects that need medical attention.
Medication Interactions
Inform your doctor about all medications, supplements, and herbal remedies you are taking. Some medications can interact dangerously with prednisone. This includes nonsteroidal anti-inflammatory drugs (NSAIDs) and certain heart medications. Your doctor can help you manage potential interactions safely.