Prednisone, a corticosteroid, often plays a crucial role in managing COPD exacerbations. Doctors typically prescribe a short course, usually 5-10 days, to reduce inflammation and improve breathing. This targeted treatment aims for quick relief, focusing on symptom control and preventing further complications.
Dosage varies depending on the severity of the exacerbation and individual patient factors. Your physician will determine the appropriate dose and schedule. Common side effects include increased appetite, mood changes, and insomnia; these are usually manageable and temporary. Always follow your doctor’s instructions precisely.
While Prednisone provides rapid relief, it’s not a long-term solution. Long-term use carries significant risks, including osteoporosis and increased susceptibility to infections. Your treatment plan will likely include other strategies, such as bronchodilators and pulmonary rehabilitation, to manage COPD effectively.
Remember to communicate openly with your healthcare provider about any concerns or side effects you experience. They can adjust your medication or treatment plan accordingly. Proactive communication ensures optimal management of your condition and minimizes potential risks associated with Prednisone use.
- Prednisone: A Quick Overview for COPD
- Understanding the Role of Prednisone in COPD Exacerbation Treatment
- Dosage and Administration
- Benefits and Potential Side Effects
- When to Seek Medical Attention
- Prednisone and Other COPD Treatments
- Long-Term Management
- Dosage and Administration of Prednisone for COPD Flare-Ups
- Tapering Schedules
- Administration
- Common Side Effects and How to Manage Them
- Common Side Effects
- Managing Side Effects: Practical Tips
- Prednisone and Other COPD Medications: Potential Interactions
- Interactions with Bronchodilators
- Interactions with Inhaled Steroids
- Interactions with Other Medications
- Managing Interactions
- When to Contact Your Doctor During Prednisone Treatment
- Other Reasons to Call Your Doctor
- Long-Term Implications and Alternative Treatment Options
Prednisone: A Quick Overview for COPD
Prednisone, a corticosteroid, reduces inflammation in your lungs, providing relief during COPD exacerbations. Doctors prescribe it for short-term use, typically 5-10 days, to manage severe symptoms like coughing, shortness of breath, and wheezing.
Dosage varies depending on your specific needs and the severity of your exacerbation; your doctor determines the correct amount. Always follow your doctor’s instructions precisely.
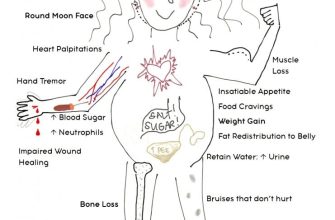
Common side effects include increased appetite, weight gain, mood changes, trouble sleeping, and increased blood sugar. Serious side effects are less common but require immediate medical attention. These may include increased risk of infection and bone thinning.
Prednisone isn’t a long-term solution for COPD. It manages flare-ups, but regular COPD management requires adherence to your prescribed inhalers and other therapies. Discuss long-term management strategies with your doctor.
Never stop taking Prednisone abruptly. Your doctor will provide guidance on tapering the dosage to minimize withdrawal symptoms.
Regular monitoring is vital while on Prednisone. Attend all scheduled appointments with your doctor for assessment and potential adjustments to your treatment plan.
Understanding the Role of Prednisone in COPD Exacerbation Treatment
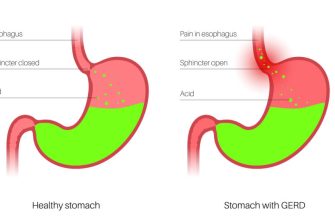
Prednisone, a corticosteroid, significantly reduces inflammation in the airways, a key factor in COPD exacerbations. It helps improve lung function and breathing, easing symptoms like shortness of breath and wheezing. Doctors prescribe it to reduce the severity and duration of flare-ups.
Dosage and Administration
Your doctor determines the appropriate dose based on your specific needs. Typical treatment involves a short course of high-dose prednisone, often tapering the amount gradually over several days to minimize side effects. Always follow your doctor’s instructions precisely regarding dosage and duration.
Benefits and Potential Side Effects
Prednisone can quickly alleviate symptoms, allowing you to breathe more easily. However, prolonged use can lead to side effects such as increased blood sugar, weight gain, mood changes, and increased risk of infection. Your doctor will monitor you closely to manage these risks. Short-term use for exacerbations generally outweighs the risks.
When to Seek Medical Attention
Contact your doctor immediately if you experience worsening shortness of breath, increased sputum production, or fever during or after treatment. These could signal a serious complication. Prompt attention ensures optimal management.
Prednisone and Other COPD Treatments
| Treatment Type | How it Works with Prednisone |
|---|---|
| Bronchodilators | Prednisone reduces inflammation; bronchodilators open airways. Used together, they provide more effective symptom relief. |
| Oxygen Therapy | Prednisone improves breathing, potentially reducing the need for supplemental oxygen, though oxygen may still be necessary. |
| Antibiotics | If infection is a cause of the exacerbation, antibiotics are prescribed. Prednisone addresses the inflammation. |
Long-Term Management
Prednisone is for acute treatment of exacerbations; it’s not a long-term solution for COPD management. Your doctor will discuss long-term strategies, such as regular medications and lifestyle adjustments, to prevent future exacerbations and improve overall lung health.
Dosage and Administration of Prednisone for COPD Flare-Ups
Your doctor will determine the appropriate prednisone dosage based on your specific needs and the severity of your COPD exacerbation. A common regimen involves a high initial dose, typically 30-60 mg daily, for several days to quickly reduce inflammation. This high dose is then gradually tapered down over 7-14 days, reducing the daily amount by a small amount (e.g., 5-10 mg) every few days, to minimize withdrawal symptoms and prevent a relapse.
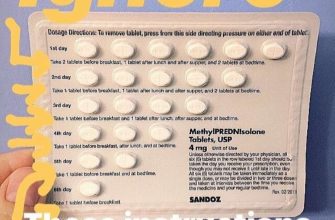
Tapering Schedules
A typical tapering schedule might look like this: 60mg for 3 days, then 50mg for 2 days, then 40mg for 2 days, then 30mg for 2 days, then 20mg for 2 days, then 10mg for 2 days, and then stopping prednisone. However, your doctor may adjust this schedule depending on your response to treatment. Always follow your doctor’s prescribed regimen carefully. They may recommend alternative schedules, especially for individuals with significant comorbidities or prior experiences with prednisone.
Administration
Prednisone is usually administered orally, as a tablet or liquid. Take the medication with food to reduce stomach upset. Drink plenty of fluids throughout the day. Consistent adherence to the prescribed schedule is key for optimal results. Remember to inform your doctor of any side effects you experience.
Common Side Effects and How to Manage Them
Prednisone, while effective for COPD exacerbations, can cause side effects. Understanding these and how to mitigate them is key to a smoother recovery.
Common Side Effects
- Increased Blood Sugar: Monitor your blood glucose levels regularly, especially if you have diabetes. Your doctor might adjust your diabetes medication. Consume smaller, more frequent meals to help manage blood sugar fluctuations.
- Fluid Retention: Reduce salt intake and drink plenty of water. Report significant swelling in your ankles, feet, or face to your doctor immediately.
- Mood Changes: Prednisone can cause irritability, anxiety, or insomnia. Maintain a regular sleep schedule, practice relaxation techniques like deep breathing, and consider talking to your doctor about managing these changes. They might suggest alternative strategies.
- Increased Appetite and Weight Gain: Choose nutritious, low-calorie foods. Increase your physical activity as tolerated to counteract caloric intake.
- Muscle Weakness: Gentle exercise, such as walking, can help. Avoid strenuous activity until your strength improves.
- Increased Risk of Infection: Practice good hygiene, avoid crowds during flu season, and report any signs of infection to your doctor promptly.
- Osteoporosis (long-term use): Discuss with your doctor strategies to maintain bone health, which might include calcium and vitamin D supplements and weight-bearing exercises.
Managing Side Effects: Practical Tips
- Follow your doctor’s instructions carefully regarding dosage and duration of treatment.
- Maintain open communication with your doctor or nurse. Report any concerning side effects immediately.
- Keep a journal to track your symptoms and how you manage them. This will help you and your doctor monitor your progress and adjust treatment as needed.
- Eat a balanced diet to support your body during recovery.
- Prioritize rest to help your body heal.
Remember, managing side effects is a crucial part of successful treatment. Don’t hesitate to contact your healthcare provider if you experience any discomfort or concerning symptoms.
Prednisone and Other COPD Medications: Potential Interactions
Always inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements, before starting prednisone. This allows them to assess potential interactions and adjust your treatment plan accordingly.
Interactions with Bronchodilators
Prednisone can enhance the effects of bronchodilators like albuterol or ipratropium, potentially leading to increased heart rate or tremors. Close monitoring of your heart rate and any side effects is necessary. Your doctor might adjust the dosage of your bronchodilator.
Interactions with Inhaled Steroids
Combining prednisone with inhaled corticosteroids (ICS) like fluticasone or budesonide increases the risk of side effects like osteoporosis and increased blood sugar. Your doctor will carefully weigh the benefits against the risks and might monitor your bone density and blood sugar levels more frequently. They may also adjust the dosage of your inhaled steroid.
Interactions with Other Medications
Prednisone interacts with many medications, including anticoagulants (like warfarin), diuretics, and certain antibiotics. This can alter their effectiveness or increase the likelihood of side effects. Discuss any potential drug interactions with your doctor or pharmacist before combining prednisone with other medications. Regular blood tests might be needed to monitor drug levels and adjust dosages if necessary.
Managing Interactions
Open communication with your healthcare team is crucial for managing potential interactions. Report any new symptoms or changes in your health immediately. Regular check-ups allow for prompt adjustments to your medication plan, ensuring the safest and most effective treatment for your COPD exacerbation.
When to Contact Your Doctor During Prednisone Treatment
Contact your doctor immediately if you experience severe side effects such as severe abdominal pain, black or bloody stools, or difficulty breathing. These could indicate serious complications.
Other Reasons to Call Your Doctor
Also, call your doctor if you notice any new or worsening symptoms, even if they seem minor. This includes increased coughing, increased shortness of breath, fever, or significant changes in your mood or sleep patterns. Report any unusual bruising or bleeding. Do not hesitate to contact them if you have concerns about your medication or its impact on your health. Consistent communication with your doctor ensures the best possible management of your COPD and your Prednisone treatment. Regular follow-up appointments are also important to monitor your progress and adjust your treatment plan as needed.
Long-Term Implications and Alternative Treatment Options
Prednisone, while effective for short-term COPD exacerbation relief, carries risks with prolonged use. Long-term prednisone use increases the chance of osteoporosis, cataracts, increased blood sugar, and weight gain. These side effects can significantly impact quality of life.
Therefore, minimizing prednisone use is crucial. Doctors often prescribe it for a limited duration, gradually tapering the dose to reduce withdrawal symptoms.
Alternative treatments focus on managing underlying COPD and preventing future exacerbations. These include:
Bronchodilators: Long-acting bronchodilators like long-acting beta-agonists (LABAs) or long-acting muscarinic antagonists (LAMAs) provide ongoing airflow improvement. A combination of LABA and LAMA is often prescribed.
Inhaled corticosteroids (ICS): These reduce inflammation in the airways, but are usually reserved for patients with frequent exacerbations or those who don’t respond well to bronchodilators alone. Careful monitoring is needed due to potential side effects, such as thrush.
Phosphodiesterase-4 inhibitors (PDE4i): These newer medications reduce airway inflammation and offer an alternative for patients who can’t tolerate ICS.
Pulmonary rehabilitation: This program includes exercise training, education, and support to improve breathing and overall fitness. It significantly reduces exacerbation rates and improves quality of life.
Oxygen therapy: For patients with low blood oxygen levels, supplemental oxygen can significantly improve symptoms and exercise capacity.
Consult your doctor to discuss a personalized treatment plan that minimizes prednisone use and maximizes long-term lung health. Regular monitoring of your COPD and adherence to your treatment plan are vital to managing your condition.