Prednisone and Plaquenil are frequently prescribed together for lupus management. Prednisone, a corticosteroid, rapidly reduces inflammation, offering immediate relief from symptoms like joint pain and fatigue. However, long-term use carries significant side effects, so doctors carefully monitor dosage and duration.
Plaquenil, a disease-modifying antirheumatic drug (DMARD), works differently. It’s used long-term to slow disease progression and prevent flares, reducing the need for high-dose Prednisone. This combination often provides the best balance between symptom control and minimizing long-term risks. Regular blood tests monitor for potential side effects from both medications, ensuring patient safety.
Remember: This information is for general knowledge only and does not substitute for professional medical advice. Individual treatment plans vary depending on disease severity, patient health, and response to medications. Always discuss your lupus management with your rheumatologist to create a personalized treatment strategy. They will assess your specific needs and adjust your medication regimen accordingly, considering potential drug interactions and monitoring for side effects.
- Prednisone and Plaquenil for Lupus: A Detailed Overview
- Prednisone: Dosage and Side Effects
- Plaquenil: Long-Term Management and Monitoring
- Understanding Lupus and its Symptoms
- Common Lupus Symptoms
- Less Common but Significant Symptoms
- Prednisone: Mechanism of Action and Lupus Treatment
- Managing Lupus Symptoms with Prednisone
- Plaquenil: Its Role in Managing Lupus Symptoms
- Combined Use of Prednisone and Plaquenil: Synergistic Effects
- Prednisone’s Rapid Action & Plaquenil’s Long-Term Effects
- Synergistic Benefits: A Powerful Combination
- Considerations & Monitoring
- Specific Recommendations
- Managing Side Effects
- Potential Side Effects of Prednisone and Plaquenil
- Monitoring and Adjusting Treatment Plans
- Long-Term Management and Lifestyle Considerations
- Managing Fatigue and Joint Pain
- Dietary Considerations
- Stress Management
- Medication Adherence
Prednisone and Plaquenil for Lupus: A Detailed Overview
Prednisone, a corticosteroid, rapidly reduces lupus symptoms like inflammation and joint pain. Doctors often prescribe it initially for symptom control. However, long-term use carries significant side effects, including weight gain, increased blood sugar, and weakened bones. Therefore, its use is typically short-term, tapering the dosage as symptoms improve.
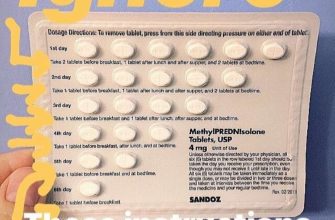
Prednisone: Dosage and Side Effects
Dosage varies depending on disease severity and individual response. Common side effects include fluid retention, mood changes, and increased risk of infections. Regular monitoring of blood pressure, blood sugar, and bone density is crucial during treatment.
Plaquenil (hydroxychloroquine), on the other hand, is a disease-modifying antirheumatic drug (DMARD). It doesn’t provide immediate relief like prednisone, but it works long-term to slow disease progression and reduce the need for higher doses of steroids.
Plaquenil: Long-Term Management and Monitoring
Plaquenil typically requires months to show noticeable effects. Common side effects are generally mild, including nausea and stomach upset. However, regular eye exams are necessary to monitor for rare but serious retinal damage.
Combining Prednisone and Plaquenil is a common treatment strategy. Prednisone addresses immediate symptoms while Plaquenil works to prevent long-term damage. This combination often allows for a quicker reduction in prednisone dosage, minimizing long-term side effects.
| Medication | Action | Typical Side Effects | Monitoring Needs |
|---|---|---|---|
| Prednisone | Rapid symptom relief | Weight gain, increased blood sugar, weakened bones, fluid retention, mood changes | Blood pressure, blood sugar, bone density |
| Plaquenil | Slows disease progression | Nausea, stomach upset | Regular eye exams |
Remember, this information is for general understanding only and doesn’t replace professional medical advice. Always consult your doctor or rheumatologist for a personalized treatment plan tailored to your specific health condition and needs.
Understanding Lupus and its Symptoms
Lupus is an autoimmune disease where your immune system mistakenly attacks healthy tissues and organs. This can lead to a wide range of symptoms, varying greatly from person to person. Some experience mild symptoms, while others face severe and debilitating challenges.
Common Lupus Symptoms
Fatigue is a frequent and often prominent symptom. Many individuals report feeling unusually tired, even after adequate rest. Joint pain and swelling (arthritis) are also common, affecting hands, wrists, and knees most often. Skin rashes, particularly a butterfly-shaped rash across the face, are characteristic but not always present. Fever, without a clear infection, is another potential sign.
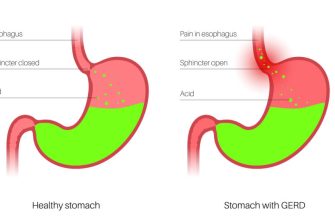
Other symptoms can include headaches, hair loss, mouth sores, and sensitivity to sunlight (photosensitivity). Lupus can also affect internal organs, causing problems with the kidneys, lungs, heart, and brain. These internal complications demand prompt medical attention.
Less Common but Significant Symptoms
Raynaud’s phenomenon, where fingers and toes change color in response to cold or stress, is seen in some lupus patients. Pleuritis (lung inflammation) and pericarditis (heart inflammation) are serious internal manifestations. Cognitive dysfunction, also known as “lupus fog,” can lead to memory problems, difficulty concentrating, and other cognitive challenges. It’s important to remember that not everyone with lupus experiences all these symptoms, and their severity varies considerably.
If you suspect you might have lupus, consult a rheumatologist for proper diagnosis and management. Early detection and treatment are key to mitigating the disease’s impact on your health and well-being.
Prednisone: Mechanism of Action and Lupus Treatment
Prednisone, a glucocorticoid, powerfully reduces inflammation by binding to glucocorticoid receptors within cells. This binding alters gene expression, decreasing the production of inflammatory molecules like cytokines and prostaglandins. This mechanism is key to its effectiveness in managing lupus symptoms.
Managing Lupus Symptoms with Prednisone
In lupus, the immune system mistakenly attacks healthy tissues. Prednisone’s anti-inflammatory action suppresses this immune response, lessening the severity of flares. It helps manage symptoms like joint pain, fatigue, and skin rashes. Doctors often prescribe Prednisone for lupus flares to quickly reduce inflammation and improve quality of life. However, long-term use carries potential side effects, so doctors carefully monitor patients and adjust dosages as needed.
Prednisone’s effects are rapid, often providing noticeable relief within days. However, it’s not a cure. Its role is primarily to manage symptoms and improve the patient’s well-being during active disease. It’s frequently used in combination with other medications, like Plaquenil, for a more comprehensive approach to lupus management. Always follow your doctor’s instructions regarding dosage and treatment duration.
Plaquenil: Its Role in Managing Lupus Symptoms
Plaquenil (hydroxychloroquine) significantly reduces lupus symptoms for many patients. It’s often a first-line treatment for managing fatigue, joint pain, and skin rashes.
Here’s how it helps:
- Reduces inflammation: Plaquenil’s anti-inflammatory properties target the underlying inflammation driving lupus symptoms.
- Protects against organ damage: Studies show it can help protect vital organs like the kidneys and heart from lupus-related damage.
- Improves quality of life: By easing symptoms, Plaquenil helps patients function better daily and participate more fully in life.
Dosage and monitoring are crucial. Your doctor will determine the appropriate dose based on your individual needs and regularly monitor your progress, including blood tests to check for potential side effects. Common side effects include nausea, stomach upset, and headache. Less common but serious side effects, such as retinal changes, necessitate regular eye exams.
Remember, Plaquenil is not a cure for lupus. It’s a disease-modifying antirheumatic drug (DMARD) that helps manage symptoms and slow disease progression. It often works best in conjunction with other medications, and your doctor will develop a personalized treatment plan.
- Regular blood tests: These help track medication effectiveness and detect potential side effects.
- Eye exams: Essential for monitoring for retinal changes.
- Open communication with your doctor: Report any new or worsening symptoms immediately.
By working closely with your rheumatologist and adhering to the prescribed treatment plan, you can optimize the benefits of Plaquenil and improve your overall lupus management.
Combined Use of Prednisone and Plaquenil: Synergistic Effects
Doctors often prescribe prednisone and Plaquenil together for lupus management. This combination leverages their distinct mechanisms to achieve better disease control.
Prednisone’s Rapid Action & Plaquenil’s Long-Term Effects
Prednisone, a corticosteroid, rapidly reduces inflammation, providing immediate relief from lupus symptoms like joint pain and fatigue. Plaquenil, however, works differently. It’s a disease-modifying anti-rheumatic drug (DMARD) that slows disease progression over time. Think of it like this: prednisone puts out the fire, while Plaquenil works to prevent future flare-ups.
Synergistic Benefits: A Powerful Combination
- Reduced Inflammation: Prednisone’s anti-inflammatory action complements Plaquenil’s long-term effects, leading to more sustained reduction in inflammation.
- Improved Organ Protection: This combination helps protect vital organs affected by lupus, such as kidneys and the heart, by reducing inflammation and limiting damage.
- Lower Prednisone Dosage: By using Plaquenil alongside prednisone, physicians can often prescribe a lower dose of prednisone, minimizing its potential side effects like weight gain and increased blood sugar.
Considerations & Monitoring
While this combination offers significant advantages, close monitoring is vital. Regular blood tests track disease activity and potential side effects. Patients should promptly report any new or worsening symptoms to their doctors.
Specific Recommendations
- Always follow your doctor’s prescribed dosage and schedule for both medications.
- Attend all scheduled follow-up appointments for monitoring and adjustments.
- Report any side effects immediately to your healthcare provider.
- Maintain open communication with your physician regarding your treatment plan.
Managing Side Effects
Both medications can cause side effects. Plaquenil’s side effects may include nausea and stomach upset, while prednisone can cause weight gain, increased blood pressure, and changes in mood. Your doctor can help manage these side effects through adjustments to your medication or other interventions.
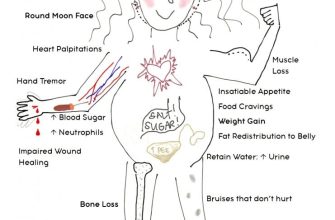
Potential Side Effects of Prednisone and Plaquenil
Both Prednisone and Plaquenil can cause side effects, though they vary in frequency and severity. Prednisone, a corticosteroid, often leads to weight gain, increased appetite, mood changes (including irritability and anxiety), high blood sugar, and increased risk of infection. Long-term use can weaken bones (osteoporosis), increase blood pressure, and cause cataracts or glaucoma.
Plaquenil, an antimalarial drug, typically produces milder side effects. Common complaints include nausea, stomach upset, and headaches. Less frequent but more serious side effects can affect the eyes (retinopathy), so regular eye exams are necessary. Skin changes, such as rash or discoloration, may also occur. Rarely, Plaquenil can damage the liver.
It’s crucial to discuss any side effects with your doctor. They can help manage these effects, possibly by adjusting medication dosage or prescribing additional medications. Early reporting allows for prompt intervention and may prevent serious complications. Remember, your doctor will weigh the benefits of these medications against the risks of side effects specific to your condition.
Monitoring and Adjusting Treatment Plans
Regular blood tests are key. Your doctor will monitor your complete blood count (CBC), liver function tests, and kidney function tests. Frequency depends on your response to treatment and any side effects. Expect tests every few months initially, possibly more often if needed.
Monitor your symptoms diligently. Keep a detailed record of fatigue levels, joint pain, skin rashes, and any other lupus symptoms. Report changes to your doctor immediately. This helps tailor your treatment plan.
Regular eye exams are crucial, particularly when taking Plaquenil. These detect potential retinal damage early. The frequency of these exams will be determined by your physician, based on your individual needs. Early detection is critical.
Dosage adjustments are common. Your doctor might increase or decrease the Prednisone dose based on your response and side effects. Plaquenil dosage changes are generally slower and less frequent. Expect open communication with your physician regarding medication adjustments.
Side effect management is vital. Report any new or worsening symptoms like weight gain, mood changes, or increased thirst. Your physician can offer solutions to mitigate these effects, possibly adjusting medication or suggesting additional therapies. Don’t hesitate to address concerns.
Treatment plans aren’t static. They adapt to your individual needs. Be proactive in your communication with your doctor to ensure optimal management of your lupus.
Long-Term Management and Lifestyle Considerations
Regularly schedule appointments with your rheumatologist for blood tests and medication adjustments. These check-ups monitor your disease activity and ensure your treatment remains effective.
Prioritize sun protection. Lupus can make your skin highly sensitive to sunlight. Use a broad-spectrum sunscreen with an SPF of 30 or higher daily, even on cloudy days, and wear protective clothing like hats and long sleeves. Limit sun exposure during peak hours (10 am to 4 pm).
Managing Fatigue and Joint Pain
Fatigue is a common lupus symptom. Get 7-9 hours of sleep each night, manage stress through relaxation techniques like deep breathing or meditation, and prioritize rest throughout the day. Gentle exercise like walking or swimming can improve energy levels but avoid overexertion. Joint pain often responds well to low-impact exercise and physical therapy. Consult with your doctor or physical therapist for personalized guidance.
Dietary Considerations
Maintain a balanced diet rich in fruits, vegetables, and lean protein. A healthy diet supports your overall health and can help manage lupus symptoms. Limit processed foods, sugary drinks, and saturated fats. Consult a registered dietitian for personalized dietary advice.
Stay hydrated by drinking plenty of water throughout the day. Adequate hydration supports kidney function, which is particularly important for people with lupus.
Stress Management
Chronic stress can worsen lupus symptoms. Practice stress-reduction techniques, such as yoga, tai chi, or mindfulness meditation. Explore stress management programs or therapy if needed.
Medication Adherence
Consistent medication adherence is key to managing lupus effectively. Develop a system to remind yourself to take your medication, such as setting alarms or using a pill organizer. Discuss any concerns or side effects with your doctor promptly.