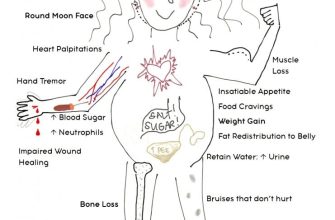
Prednisone, while a powerful anti-inflammatory medication, carries a significant risk of bone loss. Studies show that long-term use, even at moderate doses, can weaken bones, increasing the chance of fractures. This risk is particularly pronounced in postmenopausal women and individuals with pre-existing bone conditions like osteoporosis.
To mitigate this risk, prioritize regular weight-bearing exercise. Aim for at least 30 minutes most days of the week. Activities like brisk walking, jogging, and strength training directly stimulate bone growth. Simultaneously, incorporate a calcium-rich diet, focusing on dairy products, leafy greens, and fortified foods. Supplementing with calcium and vitamin D is often recommended, but always consult your doctor before starting any supplements.
Regular bone density screenings are also vital, especially if you’re on long-term prednisone therapy. These tests help monitor bone health and detect potential problems early. Your physician can recommend the appropriate frequency based on your individual risk factors and medical history. Early detection allows for timely intervention, reducing the severity of bone loss and its consequences.
Remember: Open communication with your doctor is paramount. Discuss your concerns regarding bone loss, your lifestyle choices, and any potential side effects you’re experiencing. They can adjust your medication dosage, recommend appropriate therapies, and create a personalized plan to protect your bone health while managing your underlying condition.
- Prednisone and Bone Loss: Understanding the Risk
- Factors Influencing Bone Loss Risk
- Minimizing Bone Loss Risks
- How Prednisone Affects Bone Density
- Factors Increasing Prednisone-Induced Bone Loss Risk
- Preventing and Managing Bone Loss While on Prednisone
- Lifestyle Changes for Bone Health
- Medical Interventions
- Long-Term Effects and Monitoring Bone Health
Prednisone and Bone Loss: Understanding the Risk
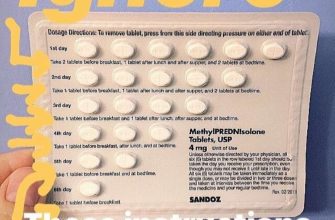
Prednisone, a powerful corticosteroid, increases your risk of osteoporosis. Long-term use, especially at high doses, significantly weakens bones, making fractures more likely. This happens because prednisone interferes with the body’s ability to absorb calcium and build new bone tissue.
Factors Influencing Bone Loss Risk
Several factors amplify this risk. Your age, pre-existing bone conditions, and overall health all play a role. Women, particularly postmenopausal women, are more susceptible. Duration of prednisone use is a key factor; the longer you take it, the higher the risk becomes. Dosage also matters – higher doses generally lead to greater bone loss.
Minimizing Bone Loss Risks
While prednisone is medically necessary for many, you can take steps to mitigate bone loss. Maintain a calcium-rich diet, including dairy products and leafy greens. Supplement with Vitamin D, crucial for calcium absorption. Regular weight-bearing exercise, such as walking or weight training, strengthens bones. Your doctor might recommend bisphosphonates or other medications to protect bone density. Regular bone density scans help monitor your bone health and allow for timely intervention.
Open communication with your doctor is paramount. Discuss your concerns, lifestyle, and medical history to develop a personalized plan to manage your bone health while on prednisone. Early detection and proactive management significantly reduce the long-term consequences.
How Prednisone Affects Bone Density
Prednisone, a powerful corticosteroid, significantly reduces bone density. This happens because it interferes with the body’s ability to absorb calcium and build new bone tissue. Specifically, prednisone suppresses the activity of osteoblasts, the cells responsible for bone formation, while simultaneously increasing the activity of osteoclasts, the cells that break down bone.
The severity of bone loss depends on several factors including the dosage of prednisone, the duration of treatment, and individual risk factors like age and pre-existing conditions. Higher doses and longer treatment periods generally lead to greater bone loss. Women, particularly post-menopausal women, are at higher risk due to reduced estrogen levels which already contribute to weaker bones.
Studies show that even short-term prednisone use can negatively impact bone mineral density. A noticeable decrease can occur within three months of starting treatment. Regular monitoring is thus vital. Your doctor might recommend bone density scans (DEXA scans) to track changes and adjust treatment accordingly.
To mitigate bone loss, your physician may recommend calcium and vitamin D supplementation. These nutrients are crucial for bone health. Weight-bearing exercise, such as walking or weight training, is also beneficial, strengthening bones and helping prevent fractures.
Bisphosphonates, a class of medications designed to slow bone loss, may be prescribed in cases of significant bone density reduction. Your doctor will carefully weigh the risks and benefits of this option based on your individual circumstances.
Remember, open communication with your doctor is key. Discuss your concerns and treatment options frankly. Proactive management can help reduce the risk of fractures and improve your long-term bone health.
Factors Increasing Prednisone-Induced Bone Loss Risk
Higher prednisone doses significantly increase bone loss risk. A daily dose exceeding 7.5mg for several months poses a considerable threat.
Duration of prednisone use is a key factor. Longer treatment periods directly correlate with greater bone density loss. Three months or more of continuous use increases the risk substantially.
Age plays a critical role. Older adults, particularly postmenopausal women, experience accelerated bone loss due to prednisone, making them a high-risk group.
Pre-existing conditions like osteoporosis or osteopenia heighten vulnerability. Individuals with these conditions should undergo rigorous monitoring during prednisone treatment.
Low calcium and vitamin D levels exacerbate the problem. Adequate intake or supplementation is crucial to mitigate bone loss during prednisone therapy. Regular blood tests to check levels are recommended.
Smoking and excessive alcohol consumption further amplify the risk. Lifestyle changes are recommended to minimize the impact of prednisone on bone health.
Genetic predisposition also contributes. A family history of osteoporosis increases the likelihood of experiencing significant bone density reduction during prednisone treatment.
Lack of weight-bearing exercise accelerates bone loss. Regular physical activity, especially weight-bearing exercises, helps strengthen bones and reduce the impact of prednisone.
Preventing and Managing Bone Loss While on Prednisone
Take a calcium and vitamin D supplement daily. Aim for 1200mg of calcium and 800-1000 IU of vitamin D. Your doctor can help determine the right dosage for you.
Engage in regular weight-bearing exercise. This includes activities like walking, jogging, dancing, hiking, and weight training. Aim for at least 30 minutes most days of the week. Bone density improves with consistent physical activity.
Maintain a healthy diet rich in fruits, vegetables, and lean protein. These provide essential nutrients for bone health. Include foods rich in Vitamin K, such as leafy greens.
Lifestyle Changes for Bone Health
Limit alcohol consumption. Excessive alcohol intake negatively impacts bone density. Moderate your alcohol intake or abstain entirely.
Quit smoking. Smoking significantly increases the risk of osteoporosis. Smoking cessation is crucial for bone health.
Medical Interventions
Discuss bisphosphonates or other bone-strengthening medications with your doctor. These medications can help slow or prevent bone loss. Your doctor will assess your individual risk and determine the best course of action.
Regularly monitor your bone density. Your doctor may recommend DEXA scans to track your bone health and adjust treatment as needed. Early detection allows for timely intervention.
Long-Term Effects and Monitoring Bone Health
Regular monitoring is key to mitigating prednisone’s impact on bone health. Schedule regular checkups with your doctor to discuss your individual risk factors and treatment plan.
Long-term prednisone use increases your risk of osteoporosis. This risk rises with higher doses and longer treatment durations. Specifically, prolonged use (over 3 months) at doses exceeding 7.5mg daily significantly elevates this risk. Fractures become a more serious concern.
- Bone Density Scans (DEXA): Your doctor might recommend these scans to measure bone density and track changes over time. These scans provide quantitative data crucial for personalized management. The frequency of scans depends on your individual risk profile and response to treatment.
- Lifestyle Adjustments: Combine medical management with proactive lifestyle changes. These include a calcium-rich diet supplemented with Vitamin D (if necessary), regular weight-bearing exercise, and smoking cessation.
- Medication Adjustments: Your doctor may adjust your prednisone dosage if possible or prescribe additional medications to protect bone health. Bisphosphonates, for example, are often used to prevent bone loss. Other options exist, and discussion with your doctor is essential to find the right approach.
Pay close attention to your body. Report any new or worsening bone pain immediately. Early detection allows for timely intervention and potentially prevents serious complications.
- Maintain a healthy weight: Obesity increases the risk of fractures.
- Engage in regular physical activity: Weight-bearing exercise strengthens bones. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Ensure adequate calcium and vitamin D intake: Dietary sources and supplements may be necessary depending on your individual needs. Your doctor can assist in determining appropriate levels.
Open communication with your healthcare provider is paramount. Actively participate in your treatment plan and don’t hesitate to ask questions. Proactive monitoring and lifestyle adjustments can significantly reduce the long-term effects of prednisone on your bones.