Need reliable information on mefloquine HCl? This guide provides specific details to help you understand its use and potential side effects. We’ll cover key aspects, offering clear explanations and avoiding jargon.
Mefloquine HCl is a medication primarily used for malaria prophylaxis. Its effectiveness varies depending on the specific strain of malaria and geographical location. Consult a physician to determine its suitability for your individual circumstances and travel plans, as resistance patterns are constantly shifting.
Common side effects include gastrointestinal issues like nausea and dizziness. Less frequent, but more serious, neuropsychiatric reactions have been reported, including anxiety, depression, and insomnia. Always report any unusual symptoms to your doctor immediately. Careful monitoring, particularly during initial use, is recommended.
Remember: Mefloquine HCl is a prescription drug. Self-medicating is dangerous. Proper dosage and monitoring are crucial for safe and effective use. Discuss potential drug interactions with your doctor before starting treatment, especially if you’re taking other medications.
This guide offers practical information, but it is not a substitute for professional medical advice. Always consult with a healthcare professional for personalized guidance and treatment before using mefloquine HCl or any medication for malaria prevention.
- Mefloquine HCl: A Detailed Overview
- Mechanism of Action and Pharmacokinetics
- Indications and Usage: When is Mefloquine Prescribed?
- Adverse Effects and Potential Risks
- Neuropsychiatric Effects
- Cardiovascular and Gastrointestinal Effects
- Dosage and Administration: Guidelines for Safe Use
- Alternatives to Mefloquine and Selection Considerations
- Factors Influencing Choice
- Comparative Table of Antimalarials
- Additional Considerations
Mefloquine HCl: A Detailed Overview
Mefloquine hydrochloride is a potent antimalarial drug, effective against Plasmodium falciparum, the most dangerous malaria parasite. It’s typically prescribed for prophylaxis (preventing malaria) in areas with chloroquine-resistant strains. Remember, consult a physician before starting any malaria prevention regimen.
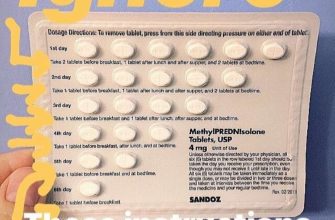
Dosage varies depending on body weight and the level of malaria risk. A doctor will determine the appropriate dosage and duration of treatment. Typical adult prophylactic doses range from 250mg weekly, beginning one or two weeks prior to exposure. Dosage adjustments are necessary for children and individuals with specific health conditions. Always strictly adhere to prescribed dosages.
Common side effects include gastrointestinal issues (nausea, vomiting, diarrhea), dizziness, and insomnia. Less common but potentially serious side effects include neurological symptoms (anxiety, depression, confusion) and cardiovascular effects (arrhythmias). If you experience any severe or unusual side effects, seek immediate medical attention.
Mefloquine interacts with several medications, including certain antidepressants and anti-anxiety drugs. It’s vital to inform your doctor about all medications and supplements you are taking before starting mefloquine. Alcohol consumption can exacerbate side effects.
Contraindications include a history of seizures, severe psychiatric disorders, and certain cardiac conditions. Pregnant or breastfeeding women should discuss the risks and benefits with their physician before considering mefloquine. Patients with a history of neuropsychiatric conditions need especially careful monitoring.
Mefloquine is typically taken orally. Store tablets in a cool, dry place, away from direct sunlight and moisture. Always follow the instructions provided by your healthcare professional and the medication leaflet. This information is for educational purposes only and does not constitute medical advice.
Mechanism of Action and Pharmacokinetics
Mefloquine hydrochloride exerts its antimalarial effect by inhibiting the parasite’s growth. Specifically, it interferes with the Plasmodium falciparum heme detoxification process. This leads to the accumulation of toxic heme, ultimately killing the parasite.
Pharmacokinetic properties are crucial for understanding mefloquine’s therapeutic use. Here’s a summary:
- Absorption: Oral bioavailability is approximately 80%, with peak plasma concentrations achieved within 1-3 hours after administration.
- Distribution: Mefloquine extensively distributes throughout the body, with high concentrations found in tissues including muscle, liver, and fat. This leads to a long half-life.
- Metabolism: Metabolism is primarily hepatic, involving oxidation and N-dealkylation.
- Elimination: Elimination is primarily biliary and renal, with a terminal elimination half-life ranging from 14 to 41 days. This long half-life allows for once-weekly dosing regimens.
Factors influencing mefloquine’s pharmacokinetics include:
- Age: Children may have faster clearance rates compared to adults.
- Renal Function: Impaired renal function can prolong the elimination half-life.
- Genetic Variation: Individual variations in metabolic enzyme activity can affect drug concentrations.
These pharmacokinetic considerations are important for determining appropriate dosage and treatment duration, minimizing potential adverse effects and ensuring optimal therapeutic outcomes.
Indications and Usage: When is Mefloquine Prescribed?
Mefloquine is primarily prescribed for the prevention of malaria caused by Plasmodium falciparum, P. vivax, P. ovale, and P. malariae. It’s particularly useful in areas with chloroquine-resistant malaria, offering protection against multiple strains.
Doctors might choose mefloquine for travelers visiting regions with high malaria risk, especially where other antimalarial drugs are less effective or not well-tolerated. This includes parts of Africa, South America, and Asia.
While prophylaxis is its main use, mefloquine can also treat uncomplicated malaria in some situations. However, its use in treatment is less common now due to the availability of other, often more effective options. The physician will assess individual patient needs and local malaria drug resistance patterns before making this determination.
Before prescribing mefloquine, your doctor will carefully consider your medical history, including any pre-existing conditions that may interact negatively with the medication. This is to minimize potential side effects and ensure the safest course of action.
Remember, mefloquine should only be taken as prescribed by a qualified healthcare professional. Self-medicating is dangerous and could lead to serious health complications. Always follow the dosage instructions precisely.
Adverse Effects and Potential Risks
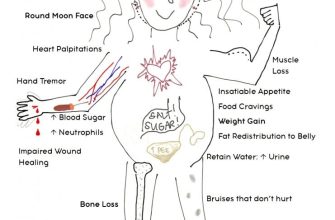
Mefloquine can cause a range of side effects, some mild and others more serious. Common side effects include nausea, dizziness, and insomnia. These usually subside as your body adjusts to the medication. However, a small percentage of users experience neurological effects, including vivid dreams, nightmares, anxiety, and depression. These can be significantly disruptive and may require immediate medical attention.
Neuropsychiatric Effects
Neuropsychiatric adverse events are a key concern with mefloquine. Reports detail psychosis, including hallucinations and paranoia, in rare instances. These serious reactions demand immediate discontinuation of the drug and prompt medical consultation. Pre-existing psychiatric conditions increase the risk of these complications. Thorough patient history, including mental health assessments, is critical before prescribing.
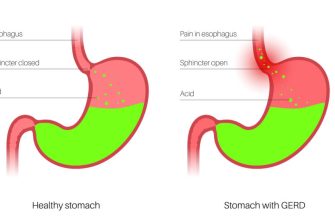
Cardiovascular and Gastrointestinal Effects
While less frequent, mefloquine can affect the cardiovascular system, causing irregular heartbeats in some individuals. Gastrointestinal issues beyond nausea, such as vomiting and diarrhea, can also occur. Severe abdominal pain warrants immediate medical evaluation. If you experience any concerning symptoms, contact your doctor immediately. Careful monitoring and open communication with your healthcare provider are crucial for managing potential risks.
Dosage and Administration: Guidelines for Safe Use
Always follow your doctor’s prescription precisely. Mefloquine hydrochloride dosage varies depending on your weight, the type of malaria you’re preventing, and your individual health.
Typical Dosage Regimens:
- Malaria Prophylaxis: A common regimen is a single dose of 250 mg weekly, starting 1-2 weeks before travel to a malaria-endemic area and continuing for 4 weeks after leaving.
- Treatment of Malaria: Dosage for treating malaria is significantly higher and determined by the specific parasite species and your individual condition. Your doctor will prescribe the appropriate dose and schedule.
Administration Instructions:
- Take mefloquine with food to minimize gastrointestinal upset.
- Swallow the tablets whole with a full glass of water. Do not crush or chew them.
- Store mefloquine at room temperature, away from moisture and direct sunlight.
Important Precautions:
- Pregnancy and Breastfeeding: Mefloquine should generally be avoided during pregnancy and breastfeeding unless the potential benefit outweighs the risk. Discuss alternatives with your doctor.
- Neuropsychiatric Effects: Mefloquine can cause serious neuropsychiatric side effects, including anxiety, depression, insomnia, and psychosis. Report any unusual mental changes immediately to your doctor.
- Cardiac Effects: Mefloquine may affect heart rhythm. Individuals with pre-existing heart conditions should exercise caution and discuss use with their physician.
- Drug Interactions: Mefloquine can interact with other medications. Inform your doctor about all medications, supplements, and herbal remedies you are taking.
- Missed Dose: If you miss a dose, take it as soon as you remember, unless it’s almost time for your next dose. Never double the dose.
Seek immediate medical attention if you experience any severe side effects. This information is for guidance only; consult your doctor for personalized advice.
Alternatives to Mefloquine and Selection Considerations
Doxycycline is a common and generally well-tolerated alternative to mefloquine. It’s effective against most strains of malaria, is readily available, and offers a convenient once-daily dosage. However, it can cause photosensitivity, so sun protection is crucial. For individuals with doxycycline allergies or contraindications, atovaquone-proguanil is a viable option providing similar efficacy.
Factors Influencing Choice
Selecting the right antimalarial requires careful assessment of individual risk factors. Travel duration, destination’s malaria prevalence and specific strains, pregnancy status, pre-existing medical conditions, and medication interactions all play a significant role. Consult a healthcare professional for personalized guidance.
Comparative Table of Antimalarials
| Medication | Dosage | Efficacy | Side Effects | Contraindications |
|---|---|---|---|---|
| Doxycycline | 100mg daily | High against *Plasmodium falciparum* and *Plasmodium vivax* | Photosensitivity, nausea, diarrhea | Pregnancy, breastfeeding, children under 8 |
| Atovaquone-Proguanil | One tablet daily | High against *Plasmodium falciparum* | Nausea, vomiting, abdominal pain | Severe liver or kidney disease |
| Primaquine | Variable, typically 15mg daily for several weeks | Effective against liver stages of malaria | Hemolytic anemia (in G6PD deficient individuals) | G6PD deficiency |
Additional Considerations
Always discuss potential drug interactions with your physician. Remember to take your medication as prescribed for the entire duration of your trip, and for several weeks afterwards as recommended, to prevent relapse. Post-travel surveillance for malaria symptoms is also recommended.