Monitor patients closely for hyperglycemia; check blood glucose levels regularly, especially in those with a history of diabetes. Report any significant increases to the physician immediately. This proactive approach helps prevent serious complications.
Assess patients for signs and symptoms of infection frequently. Prednisone suppresses the immune system, increasing susceptibility. Pay close attention to fever, chills, or any unusual changes in their condition. Early detection is crucial for prompt intervention.
Educate patients on the importance of a balanced diet rich in potassium. Prednisone can lead to hypokalemia, a condition requiring careful management. Encourage them to consume potassium-rich foods like bananas and oranges, and remind them to discuss any dietary changes with their doctor.
Carefully observe patients for fluid retention. Weight gain and edema are potential side effects. Regular weight monitoring and assessment of peripheral edema are essential parts of safe prednisone administration. Consult the physician if these symptoms worsen.
Always communicate potential adverse effects promptly to the prescribing physician. This collaborative approach ensures the patient receives optimal care and helps mitigate any risks associated with prednisone therapy. Your observations are invaluable.
Remember: This information serves as a guide; individual patient needs vary. Consult relevant drug literature and institutional policies for comprehensive guidance.
- Prednisone Nursing Implications
- Assessing for Adverse Effects
- Patient Education and Medication Management
- Monitoring for Other Complications
- Medication Interactions
- Assessing Patient’s Baseline Data
- Medication History
- Physical Assessment
- Laboratory Data
- Psychosocial Assessment
- Patient Education
- Monitoring for Adverse Effects
- Gastrointestinal Monitoring
- Infections
- Administering Prednisone Safely
- Educating the Patient on Prednisone Use
- Managing Common Side Effects
- Recognizing and Responding to Serious Complications
- Collaborating with the Healthcare Team
Prednisone Nursing Implications
Monitor patients closely for signs of infection; they’re at increased risk due to immunosuppression. Report any fever, chills, or other infection symptoms immediately.
Assessing for Adverse Effects
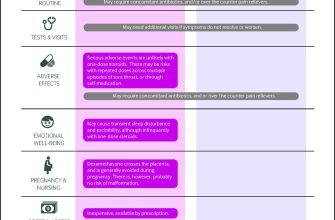
Regularly assess for common side effects like fluid retention (monitor weight and edema), hyperglycemia (check blood glucose levels), and hypertension (monitor blood pressure). Pay close attention to gastrointestinal upset; this is frequently reported. Document findings clearly and accurately.
- Fluid Retention: Weigh the patient daily, note any swelling in the extremities, and monitor intake and output.
- Hyperglycemia: Obtain blood glucose levels as ordered. Educate the patient on recognizing signs of hyperglycemia (increased thirst, frequent urination, fatigue).
- Hypertension: Monitor blood pressure at least once per shift. Adjust medication as prescribed based on response.
- Gastrointestinal Upset: Inquire about nausea, vomiting, abdominal pain, and heartburn. Administer medications as ordered to alleviate symptoms. Suggest consuming smaller, more frequent meals and avoiding spicy or acidic foods.
Patient Education and Medication Management
Educate patients on the correct administration of Prednisone, emphasizing the importance of adherence to the prescribed dosage and schedule. Remind them to avoid abrupt cessation; this can result in adrenal insufficiency.
- Explain the potential side effects and what to report to the healthcare provider.
- Stress the importance of following the prescribed dosage regimen.
- Instruct the patient to report any unusual symptoms to their doctor immediately.
- Explain the need for gradual tapering of the medication under physician supervision to prevent withdrawal symptoms.
Monitoring for Other Complications
Observe for signs of Cushing’s syndrome, such as moon face, weight gain, buffalo hump, and thin skin. Report any concerns to the healthcare provider. Regularly assess mental status changes, as mood swings and psychosis can occur. Remember to provide thorough documentation of all assessments and interventions.
Medication Interactions
Be aware of potential interactions with other medications the patient is taking. Consult drug reference guides or the physician for clarification. Always confirm the complete medication list with the patient before administering any medications.
Assessing Patient’s Baseline Data
Before initiating prednisone therapy, meticulously document the patient’s vital signs: blood pressure, heart rate, respiratory rate, and temperature. Note any pre-existing conditions, particularly diabetes, hypertension, glaucoma, osteoporosis, or peptic ulcer disease. These conditions can be exacerbated by prednisone.
Medication History
Obtain a complete medication history. Pay close attention to medications that interact with prednisone, such as nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants (like warfarin), and hypoglycemics (like insulin or oral diabetes medications). Document all medications, including over-the-counter drugs and herbal supplements.
Physical Assessment
Perform a thorough physical assessment, focusing on areas potentially affected by prednisone. Assess for signs of infection, weight, height, and body mass index (BMI). Inspect the skin for bruising or thinning. Evaluate the abdomen for tenderness. Document any pre-existing skin conditions. Note any signs of fluid retention or edema.
Laboratory Data
Review baseline laboratory values, including complete blood count (CBC), fasting blood glucose, lipid profile, and liver function tests (LFTs). These tests provide a benchmark against which to monitor potential side effects during prednisone therapy. Consider additional baseline tests based on individual patient needs and pre-existing conditions, such as bone density testing for osteoporosis risk assessment.
Psychosocial Assessment
Assess the patient’s mental status and mood. Prednisone can affect mood, causing anxiety, depression, or insomnia. Document baseline mood and any existing mental health conditions. Inquire about the patient’s support system and ability to manage their medication regimen.
Patient Education
Crucially, educate the patient about potential side effects and the importance of reporting any unusual symptoms. Provide clear instructions regarding medication administration and dosage. Discuss dietary recommendations and lifestyle adjustments to minimize potential complications. Emphasize regular follow-up appointments for monitoring.
Monitoring for Adverse Effects
Closely monitor patients for common side effects. Weight gain exceeding 2 pounds per week warrants investigation. Look for signs of fluid retention, such as edema in the ankles and legs. Regularly assess blood pressure, as prednisone can elevate it. Pay attention to changes in mood; irritability, anxiety, and depression are possible.
Gastrointestinal Monitoring
Monitor for gastrointestinal distress. This includes heartburn, abdominal pain, and nausea. Assess for signs of peptic ulcers, like black, tarry stools or bloody vomit. Encourage patients to report any digestive issues immediately.
Infections
Prednisone suppresses the immune system, increasing infection risk. Observe patients for any signs of infection, such as fever, cough, or sore throat. Promptly report any suspected infection to the physician. Encourage good hand hygiene.
Regularly check blood glucose levels, particularly in patients with diabetes, as prednisone can affect blood sugar control. Monitor for signs of hyperglycemia, such as increased thirst and frequent urination. Adjust medication accordingly, under physician guidance.
Assess bone density regularly, especially in patients at risk for osteoporosis. Prednisone can weaken bones. Consider supplemental calcium and vitamin D. Encourage weight-bearing exercise to maintain bone health.
Observe for signs of cataracts or glaucoma, particularly with prolonged use. Regular eye exams are recommended. Report any vision changes immediately.
Administering Prednisone Safely
Always follow your doctor’s prescribed dosage and schedule precisely. Never adjust the dosage without consulting your physician.
Administer Prednisone orally, with food, to minimize stomach upset. A full glass of water helps with swallowing the tablet.
- Avoid crushing or chewing tablets unless specifically instructed by your doctor or pharmacist. Some formulations are designed for delayed release.
- If you miss a dose, take it as soon as you remember, unless it’s almost time for your next dose. Never double up on doses.
- Store Prednisone at room temperature, away from moisture and direct sunlight.
Regularly monitor for side effects, including:
- Increased appetite and weight gain
- Fluid retention
- Mood changes or irritability
- Increased blood sugar levels
- Muscle weakness
- Increased risk of infection
Report any concerning side effects to your doctor immediately. Prompt reporting allows for timely intervention and adjustment of treatment.
Maintain a healthy lifestyle during Prednisone therapy. This includes:
- Eating a balanced diet.
- Engaging in regular, gentle exercise (as advised by your doctor).
- Getting adequate rest.
- Practicing good hygiene to reduce the risk of infection.
Gradually tapering off Prednisone is vital to avoid withdrawal symptoms. Always follow your doctor’s instructions for reducing the dosage. Sudden cessation can lead to serious complications.
Keep a detailed record of your medication usage and any side effects experienced. This information is valuable during follow-up appointments.
Educating the Patient on Prednisone Use
Always take Prednisone exactly as prescribed. Never adjust your dosage without consulting your doctor. Missed doses should be taken as soon as you remember, unless it’s close to your next scheduled dose. Don’t double up on doses.
Report any new or worsening symptoms to your doctor immediately. This includes, but isn’t limited to, weight gain, fluid retention, increased thirst or urination, mood changes, or vision problems.
Prednisone can weaken your immune system. Avoid contact with sick people and practice good hygiene. Discuss vaccination needs with your doctor.
Understand potential side effects. Common ones include increased appetite, insomnia, and acne. More serious side effects are less common but require immediate medical attention. Your doctor will explain these risks.
Dietary changes may be necessary. Your doctor or a registered dietitian can provide specific guidance based on your needs and potential side effects, such as increased blood sugar.
| Side Effect | Action |
|---|---|
| Increased blood sugar | Monitor blood glucose levels regularly and adjust diet as directed. |
| Muscle weakness | Engage in gentle exercise as tolerated; avoid strenuous activity. |
| Mood changes | Communicate your feelings to your doctor and family. |
| Gastrointestinal upset | Take Prednisone with food or milk. |
Prednisone’s effects don’t stop immediately when you finish your prescription. Your doctor will develop a tapering schedule to gradually reduce your dosage, minimizing withdrawal symptoms. Follow this schedule precisely.
Keep a list of all your medications and supplements. Share this list with your doctor and pharmacist. This includes over-the-counter medications and herbal remedies.
Ask questions! Don’t hesitate to contact your doctor or pharmacist if you have any concerns or uncertainties about Prednisone use.
Managing Common Side Effects
Monitor patients closely for fluid retention, reporting any significant weight gain or edema to the physician immediately. Encourage increased fluid intake unless contraindicated to help prevent dehydration, a common side effect of prednisone.
Educate patients about the increased risk of infections. Instruct them to report any signs of infection, such as fever, cough, or sore throat, without delay. Good hand hygiene and avoiding sick individuals are crucial preventive measures.
Address gastrointestinal upset by advising patients to take prednisone with food or milk to reduce stomach irritation. Antacids may be used as needed, but consult a physician for guidance.
Hyperglycemia is a potential complication. Regular blood glucose monitoring is recommended, especially for patients with diabetes or a family history of diabetes. Dietary adjustments and careful medication management are frequently necessary.
Inform patients about the potential for mood changes, including irritability, anxiety, and insomnia. Encourage open communication about these symptoms and explore strategies for coping, such as stress-reduction techniques or medication adjustments as needed by the physician.
Discuss potential osteoporosis risk with patients, particularly those with a history of bone fragility. Encourage calcium and vitamin D supplementation and weight-bearing exercises as appropriate.
Explain the possibility of increased blood pressure and the need for regular monitoring. Lifestyle changes, such as a low-sodium diet and regular exercise, along with potential medication adjustments, should be considered to mitigate this risk.
Advise patients to avoid abrupt cessation of prednisone to prevent adrenal insufficiency. Tapering the dose under medical supervision is imperative for a safe discontinuation.
Recognizing and Responding to Serious Complications
Monitor patients closely for signs of infection, including fever, chills, and increased white blood cell count. Report any suspected infection immediately to the physician. Administer antibiotics as prescribed.
Observe patients for symptoms of hyperglycemia, such as increased thirst, frequent urination, and unexplained weight loss. Regularly check blood glucose levels. Adjust insulin dosages as needed, per physician orders. Educate patients on the importance of diabetes management during Prednisone therapy.
Watch for signs of gastrointestinal distress, including nausea, vomiting, abdominal pain, and heartburn. Encourage small, frequent meals. Administer prescribed antacids or proton pump inhibitors as directed. Consider dietary modifications to minimize irritation.
Carefully assess patients for fluid retention, including edema and weight gain. Monitor vital signs regularly. Restrict sodium intake as appropriate. Consult the physician about diuretic therapy if needed.
Be vigilant for signs of Cushing’s syndrome, such as moon face, buffalo hump, and striae. These indicate prolonged high-dose corticosteroid use. Closely monitor patient progress and report any concerning changes to the prescribing physician. Discuss tapering the Prednisone dosage.
Assess patients for mood changes, including irritability, anxiety, and depression. Provide emotional support and encourage open communication. Consult mental health professionals if necessary. Closely monitor suicide risk in high-risk individuals.
Immediately report any signs of adrenal insufficiency, such as fatigue, weakness, nausea, vomiting, and hypotension. These indicate a potential crisis requiring immediate medical attention. Administer hydrocortisone as needed, per physician orders.
Educate patients about potential drug interactions and the importance of reporting all medications, including over-the-counter drugs and herbal supplements, to their physician. This reduces the risk of adverse reactions.
Collaborating with the Healthcare Team
Regularly update the physician on patient response to Prednisone, including any adverse effects. Report significant changes in blood pressure, weight, blood glucose levels, or psychological status immediately.
Closely monitor lab results with the physician, paying particular attention to electrolyte imbalances, elevated blood sugars, and signs of infection. Adjust medication or supportive care as needed based on these results.
Collaborate with the pharmacist to verify medication orders and ensure appropriate dosing and administration techniques. Discuss potential drug interactions with other medications the patient is taking.
Work with the dietitian to educate the patient on a healthy diet to manage potential side effects, such as weight gain and hyperglycemia. Encourage a balanced diet rich in fruits, vegetables, and lean protein.
Patient education is key. Team up with other healthcare professionals, such as social workers or physical therapists, to provide comprehensive support addressing the patient’s physical and emotional needs resulting from Prednisone therapy and its side effects.
Communicate proactively with the patient and their family. Clearly explain the medication’s purpose, potential side effects, and the importance of adherence to the prescribed regimen. Provide contact information for any questions or concerns.