For poison ivy rashes causing significant discomfort, Prednisone can provide rapid relief. This oral corticosteroid reduces inflammation, itching, and swelling, offering faster symptom control than many topical treatments.
A doctor typically prescribes a short course, usually lasting 7-10 days. The dosage depends on the severity of your reaction; expect your physician to tailor the prescription to your individual needs. Remember, Prednisone is a potent medication, so follow the prescribed dosage precisely and avoid abrupt cessation.
While Prednisone offers quick relief, it’s not a long-term solution. The underlying allergic reaction still needs addressing. Combine Prednisone with meticulous washing of affected areas (use soap and cool water immediately after exposure) and consider topical corticosteroids or calamine lotion for ongoing management. Always consult a doctor about your specific situation, especially with severe reactions or pre-existing health conditions.
Important Note: Prednisone has potential side effects, including increased blood sugar, insomnia, and increased appetite. Discuss any concerns with your physician before starting treatment. They can monitor for side effects and make adjustments as needed.
- Prednisone in Poison Ivy Treatment: A Detailed Guide
- What is Poison Ivy and How Does it Cause a Reaction?
- Understanding Prednisone: Its Mechanism and Uses
- Prednisone’s Role in Treating Poison Ivy
- Beyond Poison Ivy: Other Uses
- When is Prednisone Necessary for Poison Ivy?
- Factors influencing Prednisone use:
- Alternatives to Prednisone:
- Dosage and Administration of Prednisone for Poison Ivy
- Potential Side Effects of Prednisone Treatment
- Common Side Effects
- Less Common, But Important Side Effects
- Managing Side Effects
- Alternative Treatments for Poison Ivy: When Prednisone Isn’t Ideal
- Over-the-Counter Options
- Natural Remedies
- When to See a Doctor
- Important Note
- Prednisone and Other Medications: Potential Interactions
- Seeking Medical Advice: When to Consult a Doctor
Prednisone in Poison Ivy Treatment: A Detailed Guide
Prednisone, a corticosteroid, reduces inflammation and itching associated with poison ivy. Your doctor might prescribe it for severe cases with widespread rashes or significant swelling.
Oral prednisone typically comes as a tablet or liquid. Dosage depends on the severity of your reaction and your doctor’s assessment. Common regimens involve a short course – perhaps five to ten days – with gradually decreasing dosages to minimize withdrawal effects. Never alter your prescribed dosage without consulting your physician.
Expect potential side effects like increased appetite, weight gain, insomnia, and mood changes. These usually subside once you stop taking the medication. More serious side effects are rare but require immediate medical attention.
Prednisone doesn’t cure poison ivy; it manages symptoms. Combining it with other treatments, like calamine lotion for itching relief or cool compresses, often improves results. Good hygiene is critical: wash thoroughly after any potential exposure.
Before starting prednisone, inform your doctor about any pre-existing conditions, particularly diabetes, high blood pressure, or glaucoma, as it can exacerbate these. Also disclose any medications you are currently taking to avoid potential drug interactions.
Follow your doctor’s instructions carefully. Regular check-ups help monitor your progress and manage potential side effects. Remember: Prednisone isn’t a first-line treatment for mild poison ivy; home remedies may suffice. Seek medical advice if your symptoms worsen or don’t improve.
What is Poison Ivy and How Does it Cause a Reaction?
Poison ivy is a plant containing urushiol, an oily resin that causes allergic contact dermatitis in most people. Direct contact with any part of the plant – leaves, stems, roots, or even dead plant material – can trigger a reaction.
Urushiol penetrates the skin easily. It isn’t the plant’s sap that directly irritates your skin, but rather your body’s immune system reacting to urushiol. Once inside the skin, urushiol binds to skin proteins, creating an antigen which your immune system recognizes as a foreign invader. This causes your body to produce an inflammatory response, resulting in the characteristic itchy rash.
The severity of the reaction depends on several factors: the amount of urushiol exposure, your individual sensitivity, and the area of skin affected. Some individuals are highly sensitive, experiencing a strong reaction even from minimal contact, while others show only a mild response or none at all.
| Factor | Impact on Reaction |
|---|---|
| Urushiol Concentration | Higher concentration leads to more severe reaction. |
| Individual Sensitivity | Pre-existing allergies and genetic predisposition influence response. |
| Area of Exposure | Larger affected areas result in more discomfort and potential complications. |
The rash usually appears 12 to 48 hours after exposure, presenting as redness, swelling, intense itching, and blisters. It can spread if urushiol comes into contact with other areas of your body, for example, if you touch your face after touching an affected area. The rash typically resolves within two to three weeks without treatment, although severe cases may require medical intervention.
Understanding Prednisone: Its Mechanism and Uses
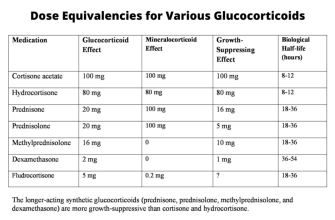
Prednisone reduces inflammation by suppressing your body’s immune response. It works by binding to specific receptors inside your cells, affecting gene expression and reducing the production of inflammatory substances like cytokines. This action significantly decreases swelling, redness, and itching–symptoms common in poison ivy reactions.
Prednisone’s Role in Treating Poison Ivy
For poison ivy, doctors prescribe prednisone to quickly control severe inflammation and allergic reactions. It’s particularly useful when the rash is extensive, causing significant discomfort or impacting daily life. It’s usually a short-term treatment, though, aimed at managing symptoms until the body’s natural healing processes can take over.
Beyond Poison Ivy: Other Uses
Prednisone treats various inflammatory conditions, including asthma, rheumatoid arthritis, and lupus. The specific dosage and treatment duration depend on the condition’s severity and the individual’s response. Your doctor will tailor the treatment plan to your needs.
When is Prednisone Necessary for Poison Ivy?
Prednisone is typically needed for severe poison ivy reactions. This means widespread rashes covering a significant portion of your body (20% or more), or reactions involving your face, genitals, or eyes. Severe swelling or blistering also warrants consideration. If you experience difficulty breathing or swallowing, seek immediate medical attention; this indicates a life-threatening allergic reaction, requiring immediate Prednisone and potentially other interventions.
Factors influencing Prednisone use:
Your doctor will consider several factors before prescribing Prednisone, including your medical history, the severity of your reaction, and the presence of any other health conditions. Pre-existing conditions like asthma or other allergies may increase the likelihood of a severe reaction, making Prednisone a more appropriate treatment. Age also plays a role; children and the elderly may be more susceptible to serious complications.
Alternatives to Prednisone:
For mild cases, topical corticosteroids like hydrocortisone cream or calamine lotion usually suffice. Oral antihistamines can help manage itching. However, if these methods prove ineffective in controlling symptoms, or if your reaction worsens, your doctor may recommend Prednisone to rapidly reduce inflammation and alleviate discomfort.
Dosage and Administration of Prednisone for Poison Ivy
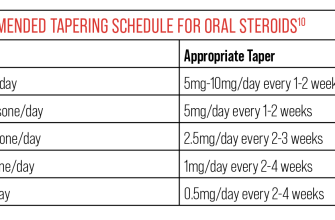
Prednisone’s dosage for poison ivy depends on the severity of your rash and your doctor’s assessment. A typical short course involves a higher initial dose, gradually decreasing over several days. This is called a tapering schedule.
Your doctor will prescribe the specific dosage and duration. However, here’s what you might expect:
- Mild cases: May require only a short course of a lower daily dose (e.g., 20-30mg daily for a few days).
- Moderate to severe cases: Might need higher initial doses (e.g., 40-60mg daily) for a longer period, gradually reducing the amount daily.
The medication is usually taken orally once daily, preferably in the morning with food to minimize stomach upset. Always follow your doctor’s instructions exactly regarding dosage, frequency, and duration of treatment.
- Never stop taking Prednisone abruptly. Always follow your doctor’s tapering schedule to prevent withdrawal symptoms.
- Report any side effects, such as stomach pain, insomnia, or increased blood sugar, to your physician immediately.
- Prednisone interacts with other medications. Inform your doctor about all medications, including over-the-counter drugs and supplements, that you’re currently taking.
Remember, this information is for general understanding and doesn’t substitute professional medical advice. Always consult your doctor or other healthcare provider for diagnosis and treatment of poison ivy, and to get a personalized prednisone prescription and plan.
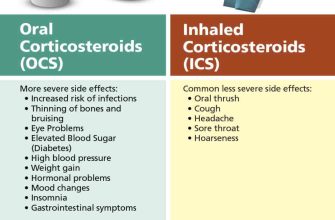
Potential Side Effects of Prednisone Treatment
Prednisone, while effective for poison ivy, carries potential side effects. These vary depending on dosage and treatment duration. Short-term use generally presents fewer issues than prolonged treatment.
Common Side Effects
Expect some common side effects like increased appetite, weight gain, trouble sleeping, mood changes (irritability, anxiety), and increased blood sugar. You might also experience fluid retention, leading to swelling in your legs or ankles. Headaches are also fairly common. These usually subside once you stop taking the medication.
Less Common, But Important Side Effects
Less frequent but still possible side effects include increased risk of infection, thinning skin, and bruising easily. Gastrointestinal issues, such as heartburn and stomach upset, can occur. In rare cases, Prednisone can cause more serious complications like increased blood pressure or cataracts. Always report any concerning symptoms to your doctor immediately.
Important Note: This information is for general knowledge and does not substitute professional medical advice. Always discuss potential risks and benefits with your doctor before starting Prednisone or any other medication.
Managing Side Effects
Your doctor can help manage side effects. Simple lifestyle adjustments, such as a balanced diet and regular exercise, can help mitigate some issues. They may also adjust your dosage or prescribe additional medication to address specific side effects.
Alternative Treatments for Poison Ivy: When Prednisone Isn’t Ideal
Prednisone effectively reduces inflammation, but it’s not suitable for everyone. Consider alternatives if you’re pregnant, breastfeeding, have diabetes, high blood pressure, or glaucoma, as prednisone can worsen these conditions. Also, long-term use carries risks.
Over-the-Counter Options
Calamine lotion soothes itching. Hydrocortisone cream (1%) provides mild anti-inflammatory relief. Apply liberally to affected areas several times daily. For more intense itching, consider oral antihistamines like diphenhydramine (Benadryl) or cetirizine (Zyrtec). Always follow package instructions.
Natural Remedies
Oatmeal baths reduce inflammation and itching. Grind colloidal oatmeal into a fine powder and add it to a lukewarm bath. Soak for 15-20 minutes. Alternatively, apply a cool compress soaked in witch hazel to the rash for temporary relief. Note: These methods offer comfort but may not cure the rash.
When to See a Doctor
Seek medical attention if your rash covers a large area of your body, you experience severe swelling, or you develop a fever. A doctor can prescribe stronger topical corticosteroids or other medications if needed. They can also diagnose secondary infections, which require specific treatment.
Important Note
Wash the affected area thoroughly with soap and water immediately after exposure to poison ivy. This step is crucial in preventing or minimizing the rash. Early treatment is key for managing poison ivy.
Prednisone and Other Medications: Potential Interactions
Always inform your doctor about all medications you are taking, including over-the-counter drugs, supplements, and herbal remedies. Prednisone can interact with numerous medications, potentially altering their effectiveness or causing side effects.
For example, Prednisone can increase blood sugar levels, so individuals with diabetes need careful monitoring when using it alongside diabetes medications like insulin or metformin. Dosage adjustments may be necessary.
Similarly, Prednisone can weaken the effects of some blood thinners like warfarin, increasing the risk of blood clots. Close monitoring of blood clotting factors is crucial in such cases.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen, when combined with Prednisone, raise the risk of stomach ulcers and bleeding. Use with caution, and consider alternatives if possible.
Prednisone can also interact with certain medications used to treat heart conditions, such as digoxin. Your physician should monitor your heart function if you are taking both medications.
Finally, remember that this information isn’t exhaustive. Discuss all your medications with your doctor or pharmacist before starting Prednisone treatment. They can help you assess potential interactions and recommend safe practices. Your safety is paramount.
Seeking Medical Advice: When to Consult a Doctor
Contact your doctor immediately if your poison ivy rash covers a large area of your body, or if you experience any of the following symptoms:
- Fever
- Swelling of the face, lips, or throat
- Difficulty breathing
- Severe blistering or weeping
- Widespread rash
- Symptoms persisting longer than two weeks despite prednisone treatment
Seek medical attention if your symptoms worsen after starting prednisone. This may signal the need for alternative treatment or a stronger medication.
Also consult your doctor if you experience any side effects from prednisone such as:
- Increased thirst or urination
- Weight gain
- Increased appetite
- Mood changes
- Sleep disturbances
- Muscle weakness
Remember, children and individuals with weakened immune systems should seek medical advice sooner than others. Prompt medical care can minimize complications and ensure rapid recovery. Don’t hesitate to contact your physician if you have any concerns.
If you have difficulty breathing, or swelling of the face, lips, or tongue, seek immediate emergency medical care. This could indicate a severe allergic reaction requiring immediate treatment.