Prednisone can significantly reduce inflammation in your airways, offering relief from an asthma cough. It’s a corticosteroid, and your doctor will likely prescribe a short course for acute flare-ups. Remember, it’s not a long-term solution for asthma management; inhalers and other preventative medications play a crucial role.
Typical dosages vary depending on your age, the severity of your cough, and your overall health. Your physician will determine the appropriate amount and duration of treatment. Always follow their instructions precisely. Incorrect usage can lead to unwanted side effects.
Common side effects include increased appetite, weight gain, mood changes, and sleep disturbances. These are usually temporary and subside once you stop taking Prednisone. However, report any unusual symptoms to your doctor immediately. Severe side effects are rare but require prompt medical attention.
Prednisone isn’t a substitute for regular asthma management. It’s a powerful tool for managing severe coughing fits but won’t address underlying asthma triggers. Continue using your prescribed inhalers and work with your doctor to create a long-term asthma action plan. This plan should include strategies for identifying and avoiding triggers to prevent future exacerbations.
Consult your doctor before starting or stopping any medication, including Prednisone. They can assess your specific situation, determine the best treatment plan, and monitor for any potential complications. This ensures your asthma is managed safely and effectively.
- When Prednisone is Prescribed for Asthma Cough
- Understanding Prednisone’s Role in Asthma Cough Treatment
- How Prednisone Works for Asthma Cough
- Important Considerations Regarding Prednisone and Asthma Cough
- Managing Side Effects and Long-Term Use of Prednisone for Asthma
- Minimizing Side Effects
- Long-Term Prednisone and Asthma Control
- Tapering Off Prednisone
- Alternative and Complementary Therapies
When Prednisone is Prescribed for Asthma Cough
Your doctor will likely prescribe prednisone for your asthma cough when other treatments haven’t adequately controlled your symptoms. This usually means your cough is severe, persistent, and interfering with your daily life. It might also be prescribed for an acute asthma exacerbation causing a significant cough.
Specifically, prednisone is useful when your cough stems from airway inflammation, a hallmark of asthma. It powerfully reduces this inflammation, easing breathing and suppressing the cough reflex. This quick-acting, anti-inflammatory effect makes it ideal for managing severe, sudden flare-ups.
Doctors consider factors like cough severity, frequency, duration, and response to other medications (like inhalers) before prescribing prednisone. They also account for your overall health and potential side effects. Prednisone isn’t a long-term solution; it’s typically a short-term treatment to control acute symptoms or severe flare-ups. Your doctor will determine the appropriate dosage and treatment duration. Regular follow-ups are necessary to monitor your progress and adjust treatment as needed.
Remember: Prednisone has potential side effects. Discuss these with your doctor to ensure informed decision-making. They’ll weigh the benefits of reducing your asthma cough against potential risks, creating a personalized treatment plan.
Always follow your doctor’s instructions precisely regarding dosage and duration of prednisone use. Never alter your prescribed treatment without consulting your physician.
Understanding Prednisone’s Role in Asthma Cough Treatment
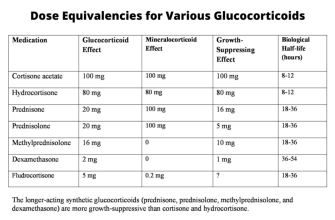
Prednisone, a corticosteroid, doesn’t directly treat the underlying cause of asthma but powerfully reduces airway inflammation. This inflammation is a key driver of the persistent cough often associated with asthma. By decreasing swelling and irritation in your airways, prednisone helps relieve coughing fits and improve breathing.
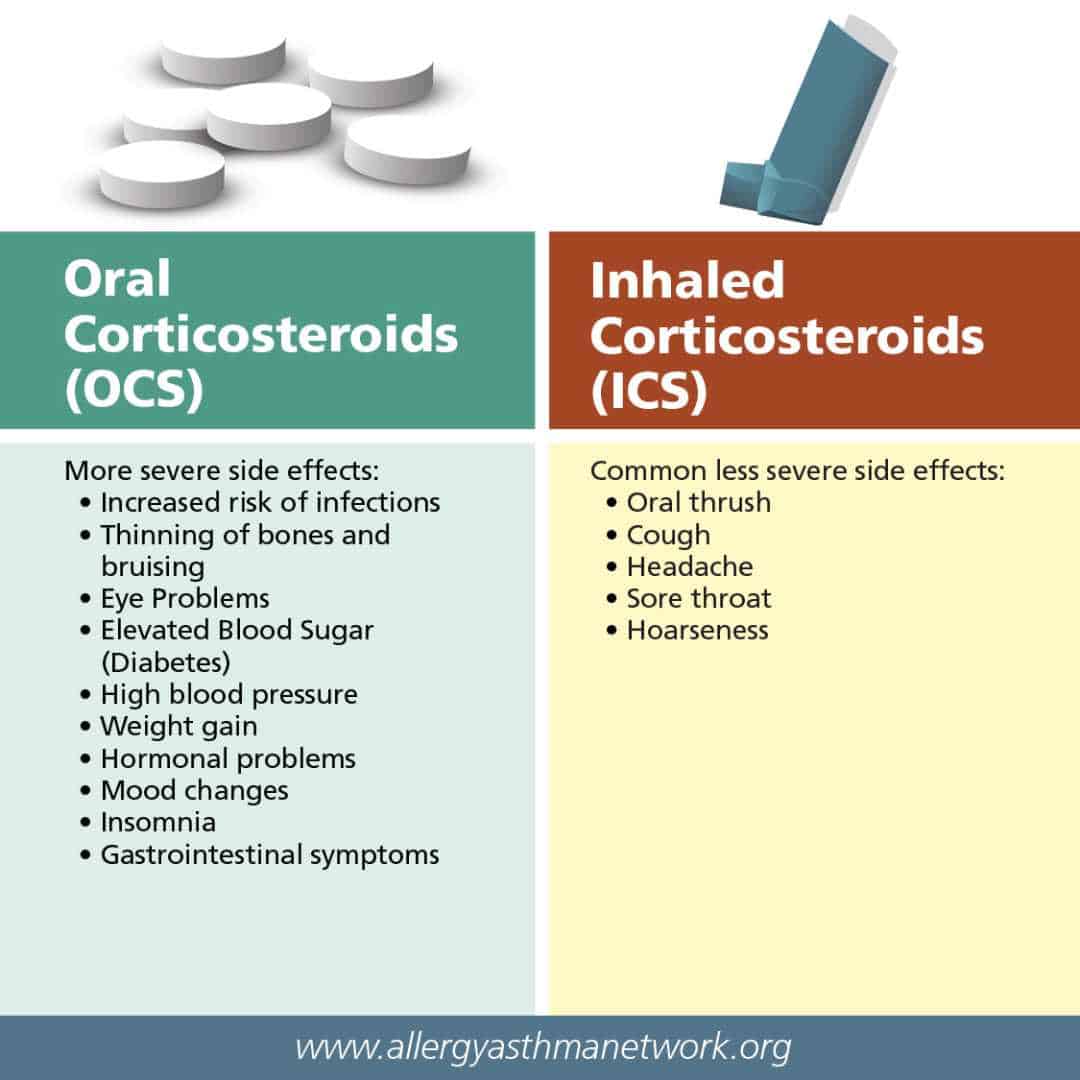
How Prednisone Works for Asthma Cough
Prednisone acts quickly, offering noticeable cough relief within hours. However, it’s important to understand that prednisone is typically used for short-term symptom management, particularly during asthma exacerbations where the cough is severe. Long-term prednisone use carries significant side effects, so your doctor will prescribe it judiciously and for specific durations. They’ll likely combine prednisone with a long-term asthma management plan, such as daily inhaled corticosteroids or bronchodilators, to prevent future attacks and minimize the need for prednisone.
Important Considerations Regarding Prednisone and Asthma Cough
Always follow your doctor’s instructions precisely regarding dosage and duration. Report any new or worsening symptoms immediately. Prednisone can interact with other medications, so inform your doctor about all the drugs you’re currently taking. Remember that prednisone doesn’t cure asthma; it addresses symptoms. Consistent use of your prescribed long-term asthma controller medication is vital for managing your condition and minimizing future coughing episodes.
Managing Side Effects and Long-Term Use of Prednisone for Asthma
Prednisone effectively controls asthma symptoms, but prolonged use carries risks. Monitor for common side effects like weight gain, increased appetite, mood changes, insomnia, and high blood pressure. Report any unusual symptoms to your doctor immediately. Regular blood pressure and blood sugar checks are crucial, particularly if you have pre-existing conditions.
Minimizing Side Effects
Your doctor can help you minimize side effects. They may prescribe the lowest effective dose and adjust the schedule to reduce exposure. Lifestyle changes, such as a balanced diet and regular exercise, also contribute to better management. Taking prednisone with food can lessen stomach upset. Discuss concerns about potential side effects openly with your healthcare provider. They can offer strategies to alleviate discomfort and help you make informed decisions.
Long-Term Prednisone and Asthma Control
Long-term prednisone use isn’t ideal for asthma. The goal is to transition to a maintenance plan with inhaled corticosteroids and other controllers as soon as possible. This reduces dependence on oral steroids and minimizes the risk of long-term side effects. Your doctor will develop a personalized plan that balances symptom control with minimizing the prednisone dosage and duration. Regular check-ups are vital to monitor your response to treatment and adjust the plan accordingly. Open communication with your doctor is key to successful long-term asthma management.
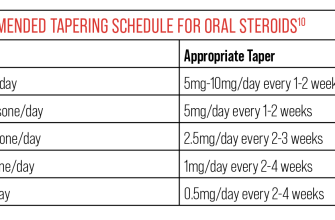
Tapering Off Prednisone
Stopping prednisone abruptly can be dangerous. Always follow your doctor’s instructions for tapering the dose gradually. This allows your body to adjust and reduces the chance of withdrawal symptoms like fatigue, muscle weakness, and joint pain. Your doctor will create a specific tapering schedule based on your individual needs and response to treatment. Be patient and follow the plan diligently.
Alternative and Complementary Therapies
Note: While prednisone remains a cornerstone of asthma treatment, some patients may benefit from exploring complementary therapies alongside their medication regimen. These could include breathing exercises, mindfulness practices, or allergy management strategies. Always discuss these options with your physician to ensure they complement and don’t interfere with your prescribed treatment.