Prednisone offers significant short-term relief for rheumatoid arthritis (RA) symptoms. Expect a reduction in inflammation and pain within days of starting treatment. However, long-term use carries risks, so your rheumatologist will likely prescribe it strategically, often in conjunction with other disease-modifying antirheumatic drugs (DMARDs).
Typical starting doses range from 5 to 60 mg daily, adjusted based on your individual response and tolerance. Common side effects include weight gain, increased appetite, mood swings, and insomnia. Open communication with your doctor about these effects is vital for managing them. Regular monitoring of blood pressure and blood sugar levels is also necessary, particularly with higher doses or prolonged treatment.
Always follow your doctor’s instructions precisely regarding dosage and duration. Sudden cessation of prednisone can lead to serious withdrawal symptoms. Your doctor will create a tapering schedule to minimize these risks, gradually reducing your dosage over several weeks or months. This careful approach ensures a smoother transition and helps prevent relapse.
Remember: Prednisone is a powerful medication. While it effectively manages RA flares, it doesn’t cure the disease. It’s a crucial tool in your RA management plan, but it’s part of a larger strategy that should include lifestyle modifications and other medications for long-term disease control.
- Prednisone in RA: A Comprehensive Guide
- What is Prednisone and How Does it Work in Rheumatoid Arthritis?
- Dosage and Administration of Prednisone for RA: What to Expect
- Adjusting Your Dosage
- Potential Side Effects
- Dosage Schedule and Administration
- Important Considerations and Monitoring
- Weaning Off Prednisone
- Common Side Effects of Prednisone: Recognizing and Managing Them
- Prednisone and Long-Term Use: Risks and Benefits
- Benefits of Long-Term Prednisone in RA
- Risks of Long-Term Prednisone Use
- Weaning Off Prednisone: A Safe and Gradual Approach
- Prednisone and Other Medications: Potential Interactions
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Diabetes Medications
- Immunosuppressants
- Blood Thinners
- Vaccines
- Heart Medications
- Antibiotics
- Calcium Channel Blockers
- Always Consult Your Doctor
- Monitoring Your Health While on Prednisone: Key Indicators
- Blood Sugar Levels
- Mood and Sleep
- Alternatives to Prednisone for RA Management
Prednisone in RA: A Comprehensive Guide
Prednisone offers rapid relief from rheumatoid arthritis (RA) symptoms, but it’s not a long-term solution. Doctors typically prescribe it for short bursts to manage flares or bridge the gap while other disease-modifying antirheumatic drugs (DMARDs) take effect.
Understanding the Dosage: Your doctor determines the correct prednisone dosage based on your individual needs and response to treatment. Common starting doses range from 5 to 60 mg daily, often tapered down gradually over weeks or months to minimize side effects.
- Tapering: Never stop prednisone abruptly. Sudden cessation can trigger adrenal insufficiency, a serious condition. Your doctor will create a specific tapering schedule.
- Monitoring: Regular blood tests monitor your progress and detect potential side effects.
Potential Side Effects: Prednisone carries side effects, varying in severity depending on dosage and duration of use. These can include:
- Weight gain
- Increased appetite
- Mood changes (irritability, anxiety, depression)
- Increased blood sugar levels
- High blood pressure
- Weakened bones (osteoporosis)
- Increased risk of infection
- Thinning skin
Managing Side Effects: Lifestyle modifications can help mitigate some side effects. A healthy diet, regular exercise, and stress management techniques are beneficial.
Long-Term Implications: Prolonged prednisone use increases the risk of serious side effects. Doctors strive for the shortest possible duration at the lowest effective dose. Your doctor will discuss long-term RA management strategies, prioritizing DMARDs for sustained disease control.
- DMARDs: Methotrexate, sulfasalazine, and leflunomide are examples of DMARDs, often used in combination with prednisone or as a replacement once the flare is controlled.
- Biologics: These targeted therapies can effectively manage RA symptoms, particularly in cases unresponsive to conventional DMARDs.
- Regular Monitoring: Consistent monitoring of your RA symptoms, and any prednisone-related side effects, is key for optimal disease management.
Communication with Your Doctor: Open communication with your rheumatologist is paramount. Report any new symptoms, concerns, or side effects promptly. They can adjust your treatment plan accordingly, ensuring you receive the best possible care.
What is Prednisone and How Does it Work in Rheumatoid Arthritis?
Prednisone is a corticosteroid medication, a powerful anti-inflammatory drug. It reduces swelling and pain by decreasing the activity of your immune system. In rheumatoid arthritis (RA), your immune system mistakenly attacks your joints, causing inflammation. Prednisone acts quickly to suppress this attack.
How it works: Prednisone binds to receptors inside your cells, affecting how your body responds to inflammation. This leads to reduced joint swelling, stiffness, and pain. It also helps improve your overall RA symptoms, allowing increased mobility and functionality.
Important Note: Prednisone is not a disease-modifying antirheumatic drug (DMARD); it doesn’t address the underlying cause of RA. It provides symptom relief, allowing time for DMARDs to take effect. Long-term use carries side effects, so your doctor will likely use it as part of a broader RA management plan. Your doctor will carefully monitor your treatment and adjust your dosage as needed.
Typical Usage: Prednisone is often prescribed for flare-ups, providing rapid symptom control. It can also be used in combination with other RA medications to manage symptoms more effectively. Doctors frequently taper prednisone dosage gradually to minimize withdrawal effects.
Potential Side Effects: These can include weight gain, increased blood sugar, high blood pressure, mood changes, and bone thinning. Your doctor will discuss these risks and monitor your health closely while you are taking prednisone.
Dosage and Administration of Prednisone for RA: What to Expect
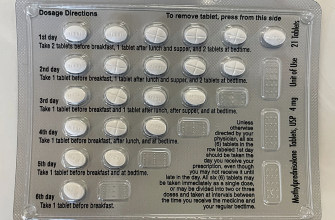
Your doctor will determine your Prednisone dosage based on your specific needs and response to treatment. Initial dosages often range from 5 to 60 mg daily, usually in a single morning dose. This helps mimic your body’s natural cortisol production cycle. Remember, always follow your doctor’s instructions precisely.
Adjusting Your Dosage
Your doctor may adjust your Prednisone dosage over time. They’ll likely start with a higher dose to control inflammation quickly, then gradually reduce it as your symptoms improve. Rapid increases or decreases are usually avoided to minimize side effects.
Potential Side Effects
Prednisone can cause several side effects, including weight gain, increased appetite, mood changes, and insomnia. More serious side effects, while less common, are also possible. Open communication with your doctor is crucial for managing these effects. They may suggest strategies for mitigating them.
Dosage Schedule and Administration
Prednisone is usually taken orally, with or without food. Your doctor will specify your daily dosage and schedule. Maintain consistency with your prescribed schedule. Skipping doses can disrupt treatment and lead to a flare-up of symptoms.
Important Considerations and Monitoring
| Factor | Recommendation |
|---|---|
| Regular Check-ups | Regular blood tests monitor your blood sugar, blood pressure, and other relevant indicators. |
| Bone Density | Long-term Prednisone use can impact bone density; your doctor might recommend monitoring or preventative measures. |
| Medication Interactions | Inform your doctor about all other medications you are taking, including over-the-counter drugs and supplements, to avoid potential interactions. |
| Tapering Off | Never stop taking Prednisone abruptly. Your doctor will create a tapering schedule to prevent withdrawal symptoms. |
Weaning Off Prednisone
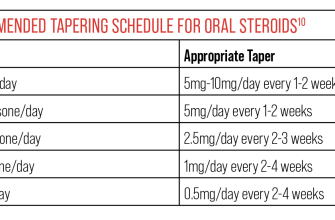
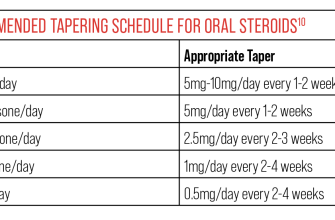
Gradually reducing your Prednisone dosage under your doctor’s supervision is essential to minimize withdrawal symptoms and prevent a relapse of RA symptoms. This process typically happens over several weeks or months, depending on your individual response to treatment and overall health.
Common Side Effects of Prednisone: Recognizing and Managing Them
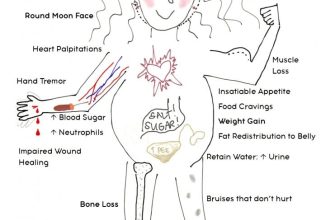
Prednisone, while effective for managing RA symptoms, can cause various side effects. Understanding these potential issues helps you proactively address them.
Weight gain is a frequent occurrence. Maintain a balanced diet and increase physical activity to mitigate this. Consult your doctor or a registered dietitian for personalized guidance.
Increased appetite is common; focus on healthy food choices to manage weight and overall health.
Mood swings are possible. Open communication with your doctor, family, and friends is vital. Consider stress-reduction techniques like yoga or meditation.
Insomnia can occur. Establish a consistent sleep schedule, create a relaxing bedtime routine, and discuss sleep aids with your doctor if needed.
Increased blood sugar levels are a concern, especially for people with diabetes. Regular blood sugar monitoring and close collaboration with your doctor are critical. Dietary adjustments may be necessary.
High blood pressure is another possible side effect. Regular monitoring and lifestyle changes, such as a low-sodium diet and regular exercise, are beneficial. Your doctor may prescribe medication to control blood pressure.
Osteoporosis risk increases with long-term prednisone use. Calcium and vitamin D supplements, along with weight-bearing exercises, can help. Your doctor may recommend bone density testing.
Muscle weakness and thinning skin are other possibilities. A balanced diet, regular exercise, and careful skin care can help manage these issues. Inform your doctor about any significant changes.
Here’s a summary of common side effects and suggested strategies:
| Side Effect | Management Strategy |
|---|---|
| Weight gain | Balanced diet, increased exercise, consult dietitian |
| Increased appetite | Focus on healthy food choices |
| Mood swings | Open communication, stress reduction techniques |
| Insomnia | Consistent sleep schedule, relaxation techniques, discuss sleep aids with doctor |
| Increased blood sugar | Regular monitoring, dietary adjustments, collaboration with doctor |
| High blood pressure | Regular monitoring, lifestyle changes, medication (if needed) |
| Osteoporosis risk | Supplements, weight-bearing exercise, bone density testing |
| Muscle weakness/thinning skin | Balanced diet, exercise, careful skin care |
Remember, this information is for general knowledge and doesn’t replace professional medical advice. Always discuss any concerns or side effects with your doctor.
Prednisone and Long-Term Use: Risks and Benefits
Doctors generally aim for the lowest effective Prednisone dose and the shortest treatment duration possible to minimize side effects. Long-term use, however, is sometimes necessary for severe RA cases. Let’s weigh the pros and cons.
Benefits of Long-Term Prednisone in RA
Prednisone effectively reduces inflammation and pain, offering significant improvements in joint function and overall quality of life for many RA patients. This can allow for greater mobility and participation in daily activities. It can also provide rapid relief during flares, preventing irreversible joint damage.
Risks of Long-Term Prednisone Use
Prolonged Prednisone use carries risks, including weight gain, increased blood sugar (potentially leading to diabetes), high blood pressure, osteoporosis (weakening of bones), cataracts, glaucoma, increased risk of infection, and mood changes (such as anxiety or depression). The severity of these side effects varies significantly between individuals, depending on factors such as dose and duration of treatment.
Bone health is a major concern. Prednisone can significantly reduce bone density, increasing the risk of fractures. Your doctor may recommend supplements like calcium and vitamin D, along with regular weight-bearing exercise, to mitigate this risk. Regular monitoring of blood pressure and blood sugar levels is also crucial. Furthermore, close attention to any changes in vision, mood, or infections is warranted.
Important Note: Prednisone should only be used under strict medical supervision. Regular blood tests and check-ups are necessary to monitor for side effects and adjust the dosage as needed. Always discuss any concerns with your rheumatologist or doctor to ensure that the benefits outweigh the risks in your specific case. Open communication is key for successful long-term management of RA with Prednisone.
Weaning Off Prednisone: A Safe and Gradual Approach
Your rheumatologist will create a personalized tapering schedule. This usually involves reducing your dose by a small amount, often 5mg or less, every few days or weeks.
Closely monitor your symptoms. Increased joint pain, stiffness, fatigue, or other RA symptoms signal the need for a slower reduction or even a temporary halt in the tapering process. Report these changes to your doctor immediately.
Maintain open communication with your healthcare team. Regularly scheduled appointments allow for adjustments to your tapering plan based on your response to the medication changes. Don’t hesitate to discuss any concerns you may have.
Consider lifestyle modifications. Maintaining a healthy diet, engaging in regular low-impact exercise, and prioritizing sufficient sleep can support your body during this transition period and help manage RA symptoms.
Expect potential side effects during withdrawal. These can include fatigue, muscle weakness, and joint pain. These are usually temporary, and your doctor can help manage them with alternative treatments or adjustments to your tapering schedule.
Never stop taking prednisone abruptly. Sudden cessation can trigger a severe relapse of your RA symptoms, potentially leading to serious health complications. Always follow your doctor’s instructions precisely.
Patience is key. The weaning process takes time and varies considerably from person to person. Be patient with yourself and celebrate your progress.
Prednisone and Other Medications: Potential Interactions
Always inform your doctor about all medications you take, including over-the-counter drugs, supplements, and herbal remedies. Prednisone interacts with many medications, potentially altering their effects or causing adverse reactions. This necessitates careful monitoring by your physician.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Combining prednisone with NSAIDs, such as ibuprofen or naproxen, increases the risk of stomach ulcers and bleeding. Your doctor might recommend alternative pain relief options. Closely monitor for any gastrointestinal discomfort.
Diabetes Medications
Prednisone can raise blood sugar levels, potentially interfering with diabetes medications. Your doctor may need to adjust your diabetes medication dosage or monitor your blood sugar more frequently. Be vigilant about monitoring your blood glucose.
Immunosuppressants
Concurrent use of prednisone and other immunosuppressants, such as methotrexate or azathioprine, increases the risk of infections. Regular monitoring for signs of infection is crucial. Report any symptoms promptly.
Blood Thinners
Prednisone can affect blood clotting, potentially interacting with anticoagulants like warfarin. This interaction requires careful monitoring of your blood clotting time by your doctor. Regular blood tests are necessary.
Vaccines
Avoid receiving live vaccines while taking prednisone, as it can weaken your immune response. Discuss vaccination plans with your rheumatologist before starting prednisone or during treatment.
Heart Medications
Prednisone may increase blood pressure. If you are taking medications for heart conditions such as hypertension, your doctor should carefully monitor your blood pressure and adjust your medication accordingly. Regular monitoring is vital.
Antibiotics
While generally safe, some antibiotics may require dosage adjustments when taken concurrently with prednisone. Consult your physician for specific guidance on antibiotics and prednisone interactions.
Calcium Channel Blockers
Simultaneous use of prednisone and calcium channel blockers may increase the risk of muscle weakness. Your doctor might suggest adjustments in your medication regime or alternative treatments.
Always Consult Your Doctor
This information is not exhaustive and does not substitute professional medical advice. Always consult your doctor or pharmacist before starting, stopping, or changing any medications, including prednisone. They can provide tailored guidance based on your specific health condition and medication history. Your doctor is your best resource.
Monitoring Your Health While on Prednisone: Key Indicators
Regularly track your weight. Prednisone can cause fluid retention and weight gain. A sudden increase of 2-3 pounds in a day warrants a call to your rheumatologist.
Monitor your blood pressure. Prednisone can elevate blood pressure. Check it daily, ideally at the same time each day. Report significant increases to your doctor immediately. Aim for consistent readings to manage this side effect effectively.
Blood Sugar Levels
Prednisone impacts blood sugar. If you have diabetes, check your glucose levels more frequently. Consult your doctor about adjusting your diabetes medication. Even without diabetes, monitor your blood sugar, especially if you experience increased thirst or frequent urination.
Mood and Sleep
Observe your mood changes. Prednisone can affect mood, potentially leading to anxiety, irritability, or depression. Report any significant shifts in your emotional state to your healthcare provider. Changes in sleep patterns, such as insomnia or excessive sleepiness, also require attention.
Pay close attention to any signs of infection. Because prednisone suppresses the immune system, infections can develop more easily. Any fever, persistent cough, or unusual skin changes should be promptly reported.
Observe your bone health. Long-term prednisone use can weaken bones. Discuss bone density testing with your doctor. Consider calcium and vitamin D supplements as your doctor recommends.
Record all symptoms and changes. A detailed log assists your doctor in monitoring your progress and making adjustments to your treatment plan as needed.
Alternatives to Prednisone for RA Management
Your rheumatologist can help you explore many options beyond prednisone. Let’s look at some key alternatives:
- Disease-Modifying Antirheumatic Drugs (DMARDs): Methotrexate is a first-line DMARD, often used alone or in combination with other medications. Sulfasalazine and hydroxychloroquine are other commonly prescribed DMARDs. These medications slow the progression of RA.
- Biologic DMARDs: These targeted therapies neutralize specific parts of your immune system contributing to inflammation. Examples include TNF inhibitors (adalimumab, etanercept, infliximab), IL-1 inhibitors (anakinra, canakinumab), and others targeting different inflammatory pathways. Your doctor will assess which biologic is best suited for your individual needs and response to treatment.
- Targeted Synthetic DMARDs (tsDMARDs): These newer medications offer a different approach to RA treatment. Examples include tofacitinib, baricitinib, and upadacitinib. They work by inhibiting specific enzymes involved in inflammation.
- Non-pharmacological approaches: Regular exercise, a balanced diet, and stress management techniques like yoga or meditation can significantly improve symptoms and quality of life. Physical therapy can help maintain joint mobility and strength.
Choosing the right alternative depends on your specific situation, including other health conditions and potential drug interactions. Your doctor will consider your RA severity, overall health, and preferences when developing a personalized treatment plan. Open communication with your rheumatologist is vital for optimal management of your RA.
Remember to discuss potential side effects and monitoring requirements with your healthcare provider for each medication option.