Prednisone elevates blood sugar primarily by reducing insulin sensitivity in your cells. This means your body becomes less responsive to insulin, hindering its ability to transport glucose from your bloodstream into your cells for energy use. Consequently, glucose levels remain higher in your blood.
Specifically, prednisone interacts with glucocorticoid receptors in your liver and muscles. This interaction stimulates gluconeogenesis – the production of new glucose from non-carbohydrate sources like amino acids and glycerol. This increased glucose production further contributes to higher blood sugar levels.
Moreover, prednisone inhibits glucose uptake in muscle tissue, adding another layer to its effect on blood sugar. This reduction in glucose uptake, coupled with increased production, creates a significant imbalance resulting in hyperglycemia.
Regular monitoring of blood glucose levels is crucial during prednisone treatment. Consult your doctor about appropriate monitoring frequency and potential adjustments to your medication or lifestyle to manage blood sugar effectively. They can guide you on managing any potential complications related to prednisone-induced hyperglycemia. Remember, proactive management is key.
Note: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for personalized guidance.
- Prednisone and Gluconeogenesis: A Detailed Look
- Enzyme Upregulation and Glucose Production
- Impact on Insulin Sensitivity
- Clinical Implications and Management
- How Prednisone Increases Gluconeogenesis in the Liver
- Prednisone’s Impact on Insulin Sensitivity and Glucose Uptake
- The Role of Insulin Resistance in Prednisone-Induced Hyperglycemia
- Managing Prednisone-Induced Hyperglycemia: Practical Strategies
- Dietary Adjustments
- Lifestyle Changes
- Medication Management
- Regular Check-ups
- Monitoring for Complications
- Hydration
Prednisone and Gluconeogenesis: A Detailed Look
Prednisone increases blood sugar levels primarily by stimulating gluconeogenesis, the process of creating glucose from non-carbohydrate sources like amino acids and glycerol. This occurs through Prednisone’s interaction with intracellular receptors. Specifically, Prednisone binds to glucocorticoid receptors, initiating a cascade of events that ultimately boosts the expression of key gluconeogenic enzymes in the liver.
Enzyme Upregulation and Glucose Production
These enzymes, including glucose-6-phosphatase and phosphoenolpyruvate carboxykinase (PEPCK), are critical for converting pyruvate and other precursors into glucose. Prednisone significantly enhances the transcription of these genes, leading to a higher concentration of active enzymes. Consequently, the liver produces and releases more glucose into the bloodstream, resulting in elevated blood sugar levels.
Impact on Insulin Sensitivity
Furthermore, Prednisone reduces the body’s sensitivity to insulin. Insulin normally signals cells to take up glucose from the blood, lowering blood sugar. Prednisone’s interference with this process diminishes insulin’s effectiveness, further contributing to hyperglycemia. This reduced insulin sensitivity is a significant factor in the development of Prednisone-induced diabetes.
Clinical Implications and Management
Understanding Prednisone’s impact on gluconeogenesis is crucial for managing its associated metabolic effects. Regular blood glucose monitoring is vital for patients on Prednisone. Lifestyle adjustments, including dietary modifications and increased physical activity, often help mitigate hyperglycemia. In some cases, antidiabetic medications may be necessary to control blood sugar levels effectively. Close collaboration with a healthcare professional is paramount.
How Prednisone Increases Gluconeogenesis in the Liver
Prednisone, a glucocorticoid, stimulates hepatic gluconeogenesis primarily through its interaction with intracellular receptors.
Increased Transcription of Gluconeogenic Enzymes: Prednisone binds to glucocorticoid receptors (GRs) within liver cells. This receptor-ligand complex translocates to the nucleus, initiating transcription of genes encoding key gluconeogenic enzymes such as glucose-6-phosphatase (G6Pase) and phosphoenolpyruvate carboxykinase (PEPCK). Higher levels of these enzymes directly boost glucose production.
Enhanced Expression of Transcription Factors: The GR-mediated transcriptional activation also involves the upregulation of specific transcription factors, like CREB (cAMP response element-binding protein), further amplifying the expression of gluconeogenic enzymes. This creates a cascade effect resulting in significantly increased glucose output.
Reduced Insulin Sensitivity: Prednisone’s impact on glucose homeostasis extends beyond direct enzyme regulation. It diminishes the liver’s sensitivity to insulin. This reduction in insulin signaling weakens insulin’s suppressive effect on gluconeogenesis, allowing the process to proceed unchecked.
Increased Glycogenolysis: Beyond gluconeogenesis, Prednisone contributes to elevated blood glucose levels by promoting glycogenolysis – the breakdown of glycogen stores into glucose – within the liver. This adds to the overall increase in circulating glucose.
Understanding these mechanisms helps explain Prednisone’s hyperglycemic effects and underscores the need for careful monitoring of blood glucose levels in patients taking this medication, particularly those with pre-existing diabetes.
Prednisone’s Impact on Insulin Sensitivity and Glucose Uptake
Prednisone reduces insulin sensitivity, hindering the body’s ability to effectively utilize glucose. This means your cells don’t respond as well to insulin, resulting in higher blood glucose levels.
The mechanism involves Prednisone’s interference with insulin receptor signaling pathways. Specifically, Prednisone can suppress insulin-stimulated glucose uptake in muscle and fat tissues. This leads to decreased glucose disposal from the bloodstream.
Additionally, Prednisone promotes gluconeogenesis, the process your liver uses to produce new glucose from non-carbohydrate sources. This further elevates blood sugar levels, exacerbating hyperglycemia.
Furthermore, Prednisone can increase insulin resistance by impacting the expression and function of key proteins involved in glucose metabolism.
Consequently, individuals taking Prednisone should closely monitor their blood sugar levels, potentially requiring adjustments in their diabetes management plan, including insulin dosage or oral hypoglycemic medications, under the guidance of their physician. Regular blood glucose monitoring is crucial for managing this side effect.
The Role of Insulin Resistance in Prednisone-Induced Hyperglycemia
Prednisone elevates blood sugar levels partly by inducing insulin resistance. This means your body’s cells become less responsive to insulin, the hormone that helps glucose enter cells for energy. Consequently, glucose accumulates in the bloodstream, leading to hyperglycemia.
This resistance stems from Prednisone’s impact on various cellular processes. It suppresses insulin signaling pathways, hindering glucose uptake. Additionally, Prednisone promotes gluconeogenesis, the liver’s production of new glucose, further increasing blood sugar.
The severity of insulin resistance varies depending on factors like dosage, duration of Prednisone use, and individual predisposition. Pre-existing conditions like obesity or family history of diabetes significantly increase susceptibility to Prednisone-induced hyperglycemia.
Managing this complication often involves close monitoring of blood sugar levels, dietary adjustments, and sometimes insulin therapy. Regular exercise can also improve insulin sensitivity and aid in glucose control. Consult your doctor to develop a personalized management plan.
Specific dietary recommendations may include reducing carbohydrate intake, particularly refined carbohydrates, and focusing on nutrient-dense foods. Your doctor can provide guidance on appropriate portions and macronutrient ratios tailored to your individual needs.
Managing Prednisone-Induced Hyperglycemia: Practical Strategies
Monitor your blood sugar regularly, aiming for at least twice daily readings, ideally before meals and before bed. Use a reliable glucose meter and keep a log to track trends.
Dietary Adjustments
- Prioritize complex carbohydrates over simple sugars. Choose whole grains, fruits, and vegetables for sustained energy release.
- Increase fiber intake. Fiber slows down glucose absorption. Aim for 25-30 grams daily.
- Spread carbohydrate intake throughout the day. Avoid large meals that can cause blood sugar spikes.
- Limit processed foods, sugary drinks, and refined carbohydrates.
- Consult a registered dietitian for personalized dietary guidance.
Lifestyle Changes
- Engage in regular physical activity. Aim for at least 150 minutes of moderate-intensity exercise per week. Even short bursts of activity help.
- Maintain a healthy weight. Excess weight can worsen insulin resistance.
- Manage stress. Stress can elevate blood sugar levels.
- Prioritize adequate sleep. Aim for 7-8 hours of quality sleep per night.
Medication Management
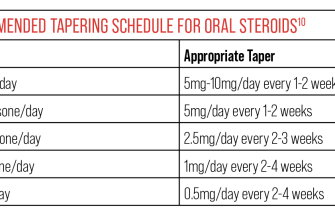
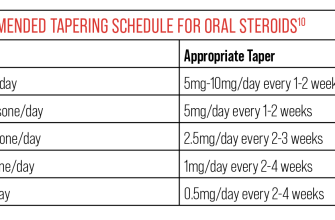
Work closely with your doctor to adjust your prednisone dosage if possible. They may explore alternative treatment options or lower your prednisone dose gradually if appropriate. Your physician might also prescribe additional medications to manage your hyperglycemia, such as metformin or insulin.
Regular Check-ups
- Schedule regular appointments with your doctor and endocrinologist to monitor blood sugar levels and adjust treatment as needed.
- Attend these appointments prepared with your blood sugar log and any questions you may have.
Monitoring for Complications
Be vigilant about symptoms of high blood sugar, including increased thirst, frequent urination, and fatigue. Promptly report any concerning symptoms to your healthcare provider. Regularly checking for long-term complications of diabetes, like kidney and eye problems, is also crucial.
Hydration
Drink plenty of water throughout the day to help your kidneys flush out excess glucose.