Need to understand the differences between azathioprine and prednisone? Prednisone, a corticosteroid, provides rapid, powerful anti-inflammatory action, making it ideal for managing acute inflammation. However, long-term use carries significant risks, including osteoporosis, cataracts, and increased susceptibility to infections. Azathioprine, on the other hand, offers a slower-acting, but often more sustainable immunosuppressive effect, better suited for long-term management of autoimmune diseases.
Consider this: Azathioprine works by inhibiting DNA synthesis, reducing the activity of your immune system gradually. This contrasts sharply with prednisone’s mechanism, which directly suppresses the inflammatory response. Doctors frequently prescribe prednisone initially to quickly control symptoms, followed by a transition to azathioprine for ongoing maintenance. This approach minimizes the long-term risks associated with high-dose corticosteroids.
Key differences lie in their side effect profiles. Prednisone’s side effects, as mentioned, can be severe and range from weight gain and mood changes to more serious complications. Azathioprine’s side effects are generally milder, including nausea, vomiting, and diarrhea, though serious complications like bone marrow suppression require careful monitoring. Always discuss these potential side effects with your physician to make an informed decision.
Ultimately, the choice depends on your specific condition, disease severity, and overall health. Your doctor will assess your individual needs and medical history to determine the most appropriate medication and dosage. Open communication with your healthcare provider is paramount to ensuring effective treatment and minimizing potential risks.
- Azathioprine vs Prednisone: A Detailed Comparison
- Mechanism of Action
- Side Effects
- Treatment Duration
- Specific Applications
- Monitoring and Management
- Conclusion
- Understanding Azathioprine’s Mechanism of Action and Uses
- Prednisone: Its Role in Autoimmune Diseases and Inflammatory Conditions
- Managing Autoimmune Conditions with Prednisone
- Addressing Inflammatory Conditions
- Important Considerations
- Comparing Side Effects: Azathioprine vs Prednisone
- Choosing the Right Medication: Factors to Consider
- Long-Term Management and Monitoring of Azathioprine and Prednisone
Azathioprine vs Prednisone: A Detailed Comparison
Choose Azathioprine for long-term disease management, while Prednisone provides rapid, albeit temporary, symptom relief. This key difference shapes their respective applications.
Mechanism of Action
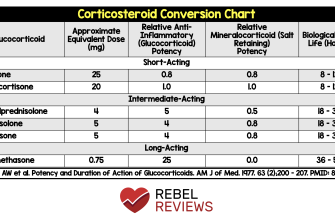
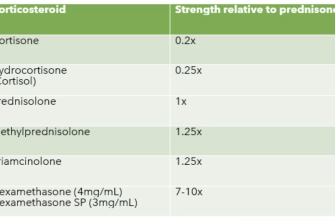
Azathioprine suppresses the immune system by interfering with DNA synthesis, reducing inflammation slowly but steadily. Prednisone, a corticosteroid, acts more rapidly by binding to intracellular receptors, leading to quick anti-inflammatory effects. This difference in speed translates to different therapeutic goals.
Side Effects
Azathioprine carries risks of infection, liver damage, and pancreatitis, requiring regular monitoring. Prednisone’s side effects, while potentially severe, often manifest more immediately and can include weight gain, increased blood sugar, and osteoporosis. Careful patient selection and monitoring are necessary for both.
Treatment Duration
Azathioprine’s prolonged action makes it ideal for chronic inflammatory conditions requiring sustained immunosuppression. Prednisone typically serves as a short-term treatment, used to control flare-ups or bridge to other therapies. Doctors carefully weigh the short-term gains against long-term risks when prescribing Prednisone.
Specific Applications
Azathioprine frequently treats autoimmune diseases like rheumatoid arthritis and inflammatory bowel disease. Prednisone finds broader use, addressing a wide spectrum of inflammatory and autoimmune conditions, as well as allergic reactions and some types of cancer. The specific disease and treatment goals dictate which medication is more appropriate.
Monitoring and Management
Regular blood tests monitor Azathioprine’s effects on the liver and blood counts. Prednisone necessitates careful observation for symptoms such as fluid retention and glucose abnormalities. Both require tailored management plans based on individual patient responses.
Conclusion
Azathioprine and Prednisone represent different approaches to managing inflammatory conditions. Azathioprine offers long-term control, while Prednisone provides rapid relief. The optimal choice hinges on the specific disease, desired outcome, and patient factors. Your doctor will make the most suitable recommendation based on your unique circumstances.
Understanding Azathioprine’s Mechanism of Action and Uses
Azathioprine suppresses the immune system by inhibiting purine synthesis, a key process in cell division and proliferation. This primarily affects rapidly dividing cells like lymphocytes, crucial players in immune responses.
Specifically, azathioprine is metabolized into 6-mercaptopurine, which interferes with DNA and RNA production. This slows down the production of immune cells, reducing inflammation and autoimmune activity.
Doctors prescribe azathioprine for various autoimmune diseases, including rheumatoid arthritis, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), and lupus. It’s also used to prevent organ rejection after transplantation.
Dosage varies based on the condition and individual patient factors. A physician carefully monitors patients on azathioprine due to potential side effects, including nausea, vomiting, diarrhea, and decreased white blood cell counts. Regular blood tests are therefore vital.
While azathioprine offers significant therapeutic benefits, it’s not a first-line treatment for all conditions. Its use is determined by a thorough assessment of the patient’s health status and the severity of their disease.
Prednisone: Its Role in Autoimmune Diseases and Inflammatory Conditions
Prednisone, a corticosteroid, powerfully suppresses the immune system, making it a cornerstone treatment for various autoimmune diseases and inflammatory conditions. It reduces inflammation by decreasing the production of inflammatory chemicals. This action provides rapid relief from symptoms, such as joint pain, swelling, and skin rashes.
Managing Autoimmune Conditions with Prednisone
Prednisone effectively treats conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease. Doctors often prescribe it to manage flare-ups or to achieve remission. However, long-term use carries risks, so doctors carefully monitor patients and adjust dosages as needed. They typically aim for the lowest effective dose to minimize side effects.
Addressing Inflammatory Conditions
Beyond autoimmune diseases, prednisone finds application in managing inflammatory conditions such as asthma, allergic reactions, and certain types of vasculitis. It significantly reduces inflammation in the airways and blood vessels, providing symptom relief. Doctors may prescribe it for short-term control of acute exacerbations or as part of a long-term management plan in severe cases, always weighing the benefits against potential adverse effects.
Important Considerations
While highly beneficial, prednisone carries potential side effects including weight gain, increased blood sugar, bone thinning, and mood changes. Regular monitoring and careful management by a physician are vital. The goal is to utilize prednisone effectively while minimizing long-term risks. Alternative treatments or a tapering schedule after symptom improvement are often implemented to reduce side effects. Open communication with your doctor is critical for effective management and ensuring your safety.
Comparing Side Effects: Azathioprine vs Prednisone
Both azathioprine and prednisone carry side effects, but their profiles differ significantly. Azathioprine, a type of immunosuppressant, more commonly causes nausea, vomiting, diarrhea, and reduced white blood cell counts, increasing infection risk. Monitor your blood counts regularly during treatment. Severe side effects are rare but include pancreatitis and liver damage; report any persistent abdominal pain or jaundice immediately.
Prednisone, a corticosteroid, frequently produces a different set of issues. Weight gain, increased appetite, mood changes, thinning skin, and increased blood sugar are common. Long-term use can also lead to osteoporosis and cataracts. Talk to your doctor about strategies to manage these side effects, such as diet modifications and supplemental calcium.
Remember: This information isn’t exhaustive. Always discuss potential side effects with your healthcare provider, who can assess your individual risk based on your health history and medication regimen. They can help you manage any side effects and make informed decisions about your treatment. Early reporting of any adverse reactions is crucial for safe medication use.
Choosing the Right Medication: Factors to Consider
Your doctor will determine the best medication for you based on several key factors. Let’s explore these carefully.
- Severity of your condition: Azathioprine is generally used for moderate to severe autoimmune diseases, while prednisone often treats milder cases or serves as a short-term, high-dose treatment for flares.
- Specific diagnosis: Certain conditions respond better to one medication than the other. Your doctor’s expertise in your specific diagnosis is vital.
- Other health conditions: Existing health issues, especially liver or kidney problems, may influence the choice, as both drugs can affect these organs. Always disclose your complete medical history.
- Drug interactions: Both azathioprine and prednisone can interact with other medications. Provide your doctor with a complete list of all your current prescriptions, over-the-counter drugs, and supplements.
- Personal preferences and lifestyle: Consider factors like ease of administration (oral vs. injection), potential side effects, and the need for regular blood tests to monitor drug levels. Open communication with your doctor is paramount.
A shared decision-making approach is best. Discuss your concerns and preferences with your physician to reach the most suitable treatment plan.
- Discuss treatment goals: What are you hoping to achieve with medication? Symptom control? Disease remission? Clear communication is key.
- Understand potential side effects: Both azathioprine and prednisone have possible adverse reactions. Your doctor can explain the risks and how to manage them.
- Plan for monitoring: Regular check-ups and blood tests are necessary to track your response to treatment and detect any problems early.
Remember, choosing the right medication is a collaborative process. Active participation in these discussions will empower you to make informed decisions about your health.
Long-Term Management and Monitoring of Azathioprine and Prednisone
Regular blood tests are key. Monitor complete blood counts (CBCs) every 2-4 weeks initially, then monthly once stable, checking for signs of bone marrow suppression. Liver function tests (LFTs) should be performed at similar intervals to detect potential liver damage, especially with azathioprine.
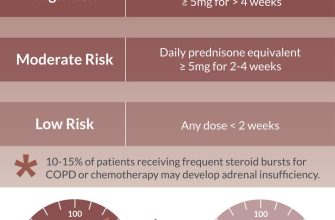
Azathioprine requires careful dosage adjustments. Start low and gradually increase based on clinical response and blood test results. Closely monitor for signs of infection, as immunosuppression is a risk. Prednisone tapering should be gradual, to avoid adrenal insufficiency. Reduce the dose incrementally, guided by the patient’s response and clinical status.
Regular check-ups with your rheumatologist are crucial. These visits allow for adjustments to medication based on the patient’s response and blood test results. Discuss any side effects experienced promptly. Common side effects of azathioprine include nausea, vomiting, and diarrhea. Prednisone can cause weight gain, increased blood sugar, and osteoporosis.
Lifestyle modifications can help manage side effects. A balanced diet and regular exercise are beneficial for mitigating prednisone-induced weight gain and improve overall health. Discuss appropriate exercise regimens with your physician, given immunosuppression. Maintain hydration by drinking plenty of fluids.
Be vigilant for warning signs. Report any unusual bleeding, bruising, persistent fatigue, fever, or jaundice to your doctor immediately. These symptoms can indicate serious complications.
Patient education is paramount. Understand your medications, their side effects, and the importance of regular monitoring. Active participation in your treatment plan improves outcomes.