Prednisone, a corticosteroid, can significantly reduce poison ivy inflammation and itching. Doctors often prescribe a short course, usually 5-10 days, depending on the severity of your rash.
For mild cases, oral prednisone might be unnecessary. However, for widespread or severe reactions – involving significant swelling, blistering, or intense discomfort – it offers fast relief. Remember to follow your doctor’s instructions precisely regarding dosage and duration.
Always consult a physician before starting prednisone, especially if you have underlying health conditions like diabetes or high blood pressure. Prednisone can interact with other medications, so inform your doctor about all your current prescriptions and over-the-counter medications. They will help you determine the appropriate dosage and monitor your progress.
Beyond prednisone, managing poison ivy involves meticulous cleaning of affected areas, using calamine lotion or hydrocortisone cream for topical relief, and keeping the rash cool and dry. This multi-pronged approach aids quicker healing and reduces discomfort.
- Treating Poison Ivy with Prednisone
- What is Poison Ivy and its Symptoms?
- When Prednisone is Necessary for Poison Ivy Treatment
- Severe Reactions Requiring Prednisone
- When to Consult a Doctor
- Alternatives to Prednisone
- How Prednisone Works to Treat Poison Ivy
- Dosage and Administration of Prednisone for Poison Ivy
- Adjusting Your Prednisone Dose
- Important Considerations
- Potential Side Effects of Prednisone for Poison Ivy
- Common Side Effects
- Less Common, But Serious, Side Effects
- Alternatives to Prednisone for Poison Ivy Treatment
- When to Seek Medical Attention for Poison Ivy
- Secondary Infection Concerns
- When Prednisone Isn’t Enough
- Helpful Guide
Treating Poison Ivy with Prednisone
Prednisone, a corticosteroid, significantly reduces poison ivy inflammation and itching. Your doctor will determine the appropriate dosage and treatment duration based on the severity of your reaction. This typically involves a short course, often 7-10 days.
Expect to see improvement within a few days. However, stopping the medication prematurely may cause symptoms to return. Always follow your doctor’s instructions.
- Dosage: This varies widely based on individual needs and the extent of the reaction. Your doctor will prescribe the correct dose.
- Side Effects: While generally safe for short-term use, potential side effects include increased appetite, weight gain, insomnia, and mood changes. Inform your doctor about any side effects you experience.
- Contraindications: Prednisone is not suitable for everyone. Individuals with certain medical conditions, such as diabetes or high blood pressure, may need careful monitoring or alternative treatment.
Prednisone is most effective when combined with other treatments. This often includes:
- Washing the affected area: Thoroughly wash the affected area with soap and water immediately after exposure to poison ivy. This helps remove urushiol oil, the allergen causing the reaction.
- Cool compresses: Applying cool compresses to the rash reduces itching and inflammation.
- Calamine lotion or hydrocortisone cream: These over-the-counter remedies can provide additional relief from itching.
Remember, prednisone manages symptoms, it doesn’t cure the rash. The rash will eventually heal on its own. For severe reactions or persistent symptoms, contact your doctor immediately.
What is Poison Ivy and its Symptoms?
Poison ivy is a plant containing urushiol, an oily resin causing allergic contact dermatitis. This means your skin doesn’t react directly to the plant itself, but to the urushiol it releases.
Exposure often leads to an itchy rash developing within a few hours to five days after contact. The rash typically appears as red bumps or blisters, sometimes forming lines or streaks where the plant brushed against your skin. These areas can swell, ooze fluid, and become quite painful.
Symptoms vary in severity depending on the amount of urushiol exposure and individual sensitivity. Some people experience mild irritation, while others develop severe reactions requiring medical treatment. The rash usually clears within two to three weeks.
Secondary bacterial infections can occur if you scratch affected areas. Watch for increased redness, swelling, pus, or fever – all signs you should seek medical attention immediately.
Remember, urushiol can spread easily. Thoroughly wash any exposed skin with soap and water as soon as possible after contact to minimize the rash’s severity. Also, wash any clothing or gear that may have come into contact with the plant separately.
When Prednisone is Necessary for Poison Ivy Treatment
Prednisone, a corticosteroid, tackles severe poison ivy reactions. Consider it when your rash is widespread (covering a significant portion of your body), intensely itchy, or significantly impacts your daily life. For instance, if the rash interferes with sleep, work, or other crucial activities, oral steroids might be beneficial.
Severe Reactions Requiring Prednisone
Widespread rashes covering more than 20% of your body usually demand prednisone. Similarly, severe blistering or facial involvement signifies a potentially serious reaction requiring medical attention and often, prednisone. Intense swelling, particularly if it affects your eyes or genitals, also warrants a doctor’s visit and likely, a prednisone prescription.
When to Consult a Doctor
Don’t hesitate to seek medical advice if home remedies fail to alleviate symptoms within a few days. Your doctor will assess your condition and determine if prednisone is the appropriate treatment. They’ll also help manage potential side effects associated with this medication.
Alternatives to Prednisone
Before considering prednisone, your doctor might suggest other treatments, such as calamine lotion, hydrocortisone cream, or oatmeal baths for milder reactions. However, if these options prove insufficient, prednisone offers a powerful solution for rapid symptom relief.
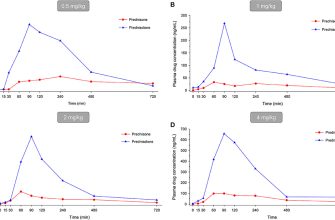
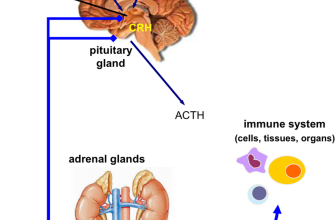
How Prednisone Works to Treat Poison Ivy
Prednisone, a corticosteroid, reduces inflammation and itching caused by poison ivy’s urushiol oil. It achieves this by suppressing your immune system’s response to the allergen. Specifically, it decreases the production of inflammatory chemicals like histamine and prostaglandins, which are responsible for the characteristic swelling, redness, and blistering.
This anti-inflammatory action quickly alleviates symptoms. You’ll notice reduced itching and swelling within days of starting treatment. The faster you begin prednisone, the better the outcome is likely to be. Dosage and treatment duration depend on the severity of your reaction; your doctor will determine the best course for you.
Keep in mind, prednisone doesn’t eliminate the urushiol oil already on your skin. Thorough washing is still crucial for preventing further exposure and spreading the rash. Prednisone only treats the body’s reaction to the oil, not the oil itself.
While generally safe when taken as prescribed, prednisone can have side effects. These can include increased appetite, weight gain, mood changes, and insomnia. Discuss any concerns with your doctor. They can help you manage potential side effects and monitor your treatment progress.
Dosage and Administration of Prednisone for Poison Ivy
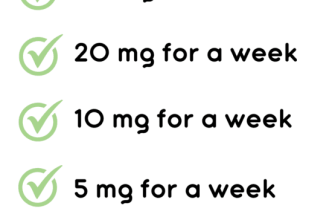
Prednisone dosage for poison ivy depends on the severity of your reaction. A doctor will determine the appropriate dose and duration of treatment. Typical oral doses range from 20 to 60 milligrams daily, often divided into multiple doses. For mild cases, a shorter course of treatment might suffice. More extensive reactions may require higher doses and a longer treatment period, potentially up to several weeks. Always follow your doctor’s instructions carefully.
Adjusting Your Prednisone Dose
Your doctor may adjust your prednisone dose based on your response to treatment. If your symptoms improve significantly, the dose might be gradually reduced. Conversely, if your symptoms worsen or don’t improve, the doctor may increase the dose. Never change your medication regimen without consulting your physician. Remember that abrupt discontinuation can lead to withdrawal symptoms. Tapering the dose under medical supervision is vital for preventing these issues.
Important Considerations
Prednisone can have side effects, including increased appetite, weight gain, insomnia, and mood changes. Inform your doctor about any side effects you experience. Long-term use can carry more significant risks, so it’s crucial to follow the prescribed course and not exceed the recommended dosage. This medication interacts with other drugs; make sure your doctor is aware of all other medications you’re taking. Regular monitoring by your doctor is necessary to ensure safe and effective treatment.
Potential Side Effects of Prednisone for Poison Ivy
Prednisone, while effective for poison ivy, can cause side effects. These vary in severity and frequency, depending on the dosage and duration of treatment.
Common Side Effects
- Increased appetite and weight gain.
- Mood changes, including irritability, anxiety, or insomnia.
- Fluid retention, leading to swelling in the face, ankles, or feet.
- Increased blood sugar levels.
- Headaches.
- Increased risk of infections.
These generally resolve once you stop taking the medication. However, it’s vital to monitor these changes and contact your doctor if they become concerning.
Less Common, But Serious, Side Effects
While less frequent, some more serious side effects warrant immediate medical attention:
- Severe allergic reactions, including difficulty breathing or swelling of the face, lips, or tongue. Seek immediate medical help.
- Muscle weakness or pain.
- Vision changes.
- Severe stomach pain.
- Increased blood pressure.
- Bone thinning (osteoporosis), particularly with prolonged use.
This list isn’t exhaustive; other side effects are possible. Always discuss potential risks with your doctor before starting prednisone. They can help you weigh the benefits against the potential drawbacks, and adjust dosage and treatment duration accordingly.
Alternatives to Prednisone for Poison Ivy Treatment
For mild poison ivy reactions, consider calamine lotion to soothe itching. Apply liberally and frequently as needed for relief.
Over-the-counter hydrocortisone cream (1%) offers topical anti-inflammatory action. Apply to affected areas following package directions. For more persistent itching, a stronger topical steroid, such as 0.5% betamethasone dipropionate, may be prescribed by your doctor.
Oral antihistamines, like diphenhydramine (Benadryl) or cetirizine (Zyrtec), can help manage the allergic reaction and reduce itching. Follow dosage instructions carefully.
Cool compresses or oatmeal baths provide soothing relief from inflammation and itching. Apply cool compresses directly to affected skin. For oatmeal baths, add colloidal oatmeal to lukewarm bathwater.
If you suspect a severe reaction, including widespread rash or difficulty breathing, seek immediate medical attention. Your doctor can assess your condition and recommend appropriate treatment.
When to Seek Medical Attention for Poison Ivy
Seek immediate medical attention if you experience a severe reaction, such as difficulty breathing or swelling of your face, lips, or throat. This indicates a potential life-threatening allergic reaction requiring immediate medical intervention.
Contact your doctor if your rash covers a large area of your body (more than 20% of your skin), especially if it’s accompanied by fever or chills. This suggests a more widespread infection requiring professional care.
Also, seek medical advice if your symptoms worsen despite home treatment, or if your poison ivy rash persists for more than two to three weeks. Persistence beyond this timeframe might indicate secondary infection or a need for additional treatment options.
Secondary Infection Concerns
Watch for signs of a secondary bacterial infection, including increased pain, pus-filled blisters, red streaks radiating from the rash, or worsening swelling. These symptoms necessitate prompt medical evaluation and likely antibiotic treatment.
When Prednisone Isn’t Enough
If your doctor prescribes prednisone but your symptoms don’t improve or you experience significant side effects from the medication, contact them immediately. They may adjust your treatment plan or offer alternative approaches.
Helpful Guide
| Symptom | Action |
|---|---|
| Difficulty breathing, facial swelling | Go to the emergency room immediately. |
| Rash covering >20% of body, fever | Call your doctor immediately. |
| Rash persists >3 weeks, worsening symptoms | Schedule an appointment with your doctor. |
| Signs of secondary infection (pus, red streaks) | Seek medical attention urgently. |
| No improvement with prednisone or side effects | Contact your doctor immediately. |