Experiencing a rash after starting Prednisone? Don’t panic. Many people develop skin reactions, ranging from mild redness to more significant eruptions. Understanding the causes and appropriate responses is key to managing discomfort and ensuring safe treatment. This article will guide you through identifying potential rash types, suggesting self-care strategies, and explaining when professional medical attention is necessary.
Prednisone rashes often manifest as hives, small red bumps, or widespread inflammation. The severity varies widely depending on individual factors like dosage and duration of Prednisone use, as well as pre-existing skin conditions. Pay close attention to symptoms like itching, swelling, or blistering, and note the exact location and appearance of the rash. Taking clear photos can be helpful for your doctor.
First-line management frequently involves adjusting the Prednisone dosage or, in some cases, switching to an alternative medication. However, you should never alter your medication regimen without consulting your physician. Simple self-care measures like cool compresses, oatmeal baths, and over-the-counter antihistamines can help alleviate itching and inflammation. For more severe reactions characterized by widespread swelling or difficulty breathing, seek immediate medical assistance.
Your doctor will conduct a thorough evaluation to determine the underlying cause of the rash and recommend the best course of action. This may involve blood tests, skin biopsies, or other diagnostic tools. Remember, open communication with your healthcare provider is crucial for successful treatment and minimizing potential risks.
- Prednisone-Induced Rash: A Comprehensive Guide
- Understanding Prednisone and its Side Effects
- Identifying Prednisone Rash: Types and Appearance
- Common Prednisone Rash Types
- Less Common, but Important, Presentations
- Severity of Prednisone Rash: Mild to Severe Reactions
- Moderate Prednisone Rash
- Severe Prednisone Rash
- When to Seek Medical Attention for a Prednisone Rash
- Treatment Options for Prednisone-Induced Rash
- Preventing Prednisone Rash: Tips and Strategies
- Dietary Adjustments
- Sun Protection
- Medication Management
- Lifestyle Changes
- Living with Prednisone Rash: Managing Symptoms and Long-Term Effects
- Prednisone Rash and Other Medications: Potential Interactions
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Warfarin (Coumadin)
- Immunosuppressants
- Antidiabetic Medications
- Potassium-Depleting Diuretics
- Cardiac Glycosides (e.g., Digoxin)
- Other Medications
- Reporting Adverse Reactions
Prednisone-Induced Rash: A Comprehensive Guide
See your doctor immediately if you develop a rash while taking prednisone. This is crucial for proper diagnosis and treatment.
Prednisone rashes vary widely in appearance. They can range from mild redness and itching to severe blistering. Some rashes manifest as hives or small, red bumps. Others present as larger, inflamed patches of skin.
Several factors influence rash severity, including dosage, duration of prednisone use, and individual sensitivity. Higher doses and longer treatment periods increase the risk of a more serious reaction.
Treatment depends on the rash’s severity. Mild rashes might require only discontinuation of prednisone and application of a topical corticosteroid cream. More severe reactions may need oral antihistamines, stronger topical treatments, or even a different medication to replace prednisone.
Remember: Never stop prednisone abruptly without consulting your physician. Sudden cessation can lead to serious health complications.
Prevention isn’t always possible, but minimizing prednisone exposure is key. Your doctor can discuss alternative treatments or lower dosages if appropriate.
Prompt medical attention is paramount. Early intervention improves the chances of a favorable outcome and minimizes potential complications.
Note: This information serves as guidance; it does not replace professional medical advice. Always consult your doctor for diagnosis and treatment.
Understanding Prednisone and its Side Effects
Prednisone, a corticosteroid, powerfully reduces inflammation but carries potential side effects. Skin reactions, like rashes, are common. The severity varies; some experience mild redness, others more significant eruptions.
Weight gain is another frequent side effect, often due to fluid retention and increased appetite. Regular monitoring of weight and diet is advised. Increased blood sugar levels are also possible, posing a risk for individuals with diabetes or predisposed to it. Regular blood glucose checks are necessary for those at risk.
Mood changes are a concern; some report irritability, anxiety, or even depression. Open communication with your doctor is vital if you experience such shifts. Osteoporosis risk increases with prolonged use due to decreased bone density. A balanced diet rich in calcium and vitamin D, along with regular exercise, can help mitigate this risk. Your doctor might recommend bone density testing.
High blood pressure is also a possible side effect. Regular blood pressure monitoring is important, particularly if you have pre-existing hypertension. Stomach ulcers are a less common but serious risk. Your physician might suggest protective medications. Always inform your doctor of any existing conditions before starting Prednisone.
Remember, these are potential side effects, not guaranteed outcomes. The likelihood and severity depend on factors like dosage, duration of use, and individual sensitivity. Consistent communication with your healthcare provider allows for close monitoring and adjustments as needed.
Identifying Prednisone Rash: Types and Appearance
Prednisone rashes manifest in various ways. Recognizing the different types is key to appropriate management. Look for these common presentations:
Common Prednisone Rash Types
| Rash Type | Appearance | Additional Notes |
|---|---|---|
| Maculopapular Rash | Flat, red spots (macules) or raised, red bumps (papules), often widespread. May be itchy. | Often appears on the torso, arms, and legs. |
| Purpuric Rash | Red or purple spots or patches that don’t blanch (don’t turn white when pressed). Can indicate a more serious reaction. | Seek medical attention immediately if you observe this type. |
| Acneiform Rash | Looks like acne – pimples, pustules, and sometimes cysts. | Usually appears on the face, chest, and back. |
| Erythematous Rash | Generalized redness of the skin. | Can be accompanied by warmth and swelling. |
Less Common, but Important, Presentations
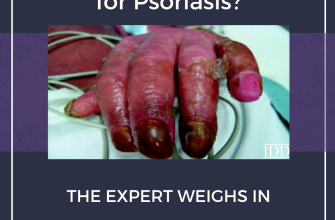
Less frequent, but still possible, are reactions resembling psoriasis or other skin conditions. These can mimic existing conditions, so a doctor’s diagnosis is particularly important. If your rash shows signs of blistering, significant swelling, or severe itching, seek immediate medical attention. Accurate identification ensures proper treatment and helps avoid complications.
Severity of Prednisone Rash: Mild to Severe Reactions
Prednisone rashes vary significantly in appearance and intensity. Mild reactions often present as small, red, itchy bumps or hives. These typically appear on the torso or extremities. Treatment might involve topical corticosteroids or antihistamines, providing sufficient relief for many individuals. Careful monitoring is advised, as even mild reactions can worsen.
Moderate Prednisone Rash
Moderate rashes involve larger, more widespread areas of redness and inflammation. Blistering or scaling might occur, and itching intensifies significantly. Oral corticosteroids (a higher dose of prednisone or a different steroid medication) or stronger topical treatments are usually prescribed. Close medical supervision becomes crucial during this phase to prevent complications.
Severe Prednisone Rash
Severe reactions necessitate immediate medical attention. Symptoms include widespread blistering, significant swelling, fever, and potential difficulty breathing. These reactions can indicate a serious allergic response and may require hospitalization for intravenous steroids and other supportive care. In rare cases, Stevens-Johnson syndrome or toxic epidermal necrolysis, potentially life-threatening conditions, can develop. Early intervention is paramount to minimizing damage and improving prognosis.
When to Seek Medical Attention for a Prednisone Rash
Contact your doctor immediately if your rash is accompanied by difficulty breathing or swelling of your face, lips, or tongue. These are signs of a severe allergic reaction that requires immediate medical care.
Seek medical attention if your rash rapidly spreads, becomes increasingly painful, or develops blisters or oozing sores. Severe itching that disrupts your sleep or daily activities also warrants a doctor’s visit.
If you experience fever or chills alongside the rash, contact your doctor. This could indicate a more serious infection.
Don’t hesitate to call your doctor if the rash doesn’t improve or worsens after a few days, even if it seems mild. Early intervention can often prevent complications.
Your doctor can accurately assess your condition and provide appropriate treatment. Always follow their recommendations regarding your medication and rash management.
Treatment Options for Prednisone-Induced Rash
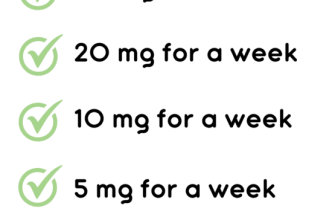
First, discuss tapering or discontinuing prednisone with your doctor. This is often the primary treatment strategy. A gradual reduction in dosage minimizes withdrawal symptoms and may resolve the rash.
If prednisone reduction isn’t sufficient, your doctor might prescribe antihistamines like diphenhydramine or cetirizine to alleviate itching. These are readily available and often provide quick relief.
Topical corticosteroids, applied directly to the rash, can reduce inflammation and itching. Your doctor can guide you on the appropriate strength and application method.
For more severe cases, oral corticosteroids may be considered, though a different medication might be used. This option should be discussed with your physician to assess risks and benefits.
In rare instances, immunosuppressants might be needed. This is generally reserved for severe, unresponsive cases and should be determined by a medical professional considering potential side effects.
Cool compresses can soothe inflamed skin, offering temporary relief from itching and discomfort. This simple home remedy can be used alongside other treatments.
Oatmeal baths can also provide soothing relief. Colloidal oatmeal products are widely available at pharmacies.
Maintaining good skin hygiene is important. Gentle cleansing with fragrance-free soaps prevents further irritation. Avoid harsh scrubs or scented products.
Always consult your doctor before starting any new treatment for a prednisone-induced rash. They can provide personalized recommendations based on your specific needs and medical history.
Preventing Prednisone Rash: Tips and Strategies
Drink plenty of water. Hydration helps your body process the medication and flush out potential irritants.
Apply a cool compress to any itchy areas. This soothes inflammation and provides temporary relief. Avoid scratching, as this can worsen the rash.
Consider using gentle, fragrance-free moisturizing lotions. This keeps your skin hydrated and prevents dryness, a common trigger for rashes.
Dietary Adjustments
Minimize processed foods, red meat, and alcohol. These can exacerbate inflammation throughout the body, potentially worsening skin reactions.
Increase your intake of fruits and vegetables rich in antioxidants. These support your immune system and help protect your skin.
Sun Protection
Use a broad-spectrum sunscreen with an SPF of 30 or higher. Prednisone can make your skin more sensitive to sunlight, increasing the risk of sunburn and rash aggravation.
Wear protective clothing when spending time outdoors, especially during peak sun hours.
Medication Management
Take prednisone exactly as prescribed by your doctor. Do not adjust the dosage without consulting them.
Report any skin changes or other side effects to your doctor immediately. Early intervention is key to managing potential complications.
Lifestyle Changes
Manage stress levels. Stress can trigger or worsen skin conditions. Techniques like meditation or yoga can help.
Maintain good hygiene. Showering daily with mild soap can help keep your skin clean and prevent infections.
Living with Prednisone Rash: Managing Symptoms and Long-Term Effects
Apply cool compresses to the affected area for 15-20 minutes several times a day to reduce inflammation and itching. This simple step offers immediate relief.
Take lukewarm showers or baths instead of hot ones. Avoid harsh soaps and scrubbing. Gentle cleansing is key to preventing further irritation.
Consider over-the-counter hydrocortisone cream (1%) or calamine lotion to soothe the rash. Always follow product instructions carefully. These can provide localized relief from itching.
Loose, breathable clothing minimizes friction and prevents further irritation. Cotton fabrics are preferable to synthetics.
- Avoid tight-fitting clothing, especially around the affected areas.
- Choose natural fibers over synthetic fabrics.
Keep your skin hydrated by drinking plenty of water and using a fragrance-free moisturizer. Adequate hydration aids skin healing.
Monitor the rash closely. If it worsens significantly, spreads rapidly, or is accompanied by fever or other symptoms, seek immediate medical attention. Prompt medical intervention is vital for severe cases.
- Document the rash’s progression with photos.
- Note any changes in size, color, or associated symptoms.
- Contact your doctor promptly for any concerning developments.
Long-term effects are rare, but in some cases, persistent skin dryness or hyperpigmentation may occur after the rash resolves. Maintaining good skin hydration habits helps mitigate these potential effects. Regular moisturizing is crucial for long-term skin health after steroid treatment.
Consult your doctor or dermatologist about potential long-term management strategies if you experience persistent skin issues. They can provide personalized advice and treatment options.
Prednisone Rash and Other Medications: Potential Interactions
Always inform your doctor about all medications you’re taking, including over-the-counter drugs, supplements, and herbal remedies. This helps prevent potentially harmful drug interactions.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Combining prednisone with NSAIDs like ibuprofen or naproxen increases your risk of stomach ulcers and bleeding. Your doctor might recommend alternative pain relievers.
Warfarin (Coumadin)
Prednisone can alter how your body processes warfarin, a blood thinner. This interaction requires close monitoring of your blood clotting levels. Regular blood tests are necessary.
Immunosuppressants
Concurrently using prednisone and other immunosuppressants, such as azathioprine or cyclosporine, significantly raises your risk of infections. Your doctor will carefully weigh the benefits against these increased risks.
Antidiabetic Medications
- Prednisone can elevate blood sugar levels, potentially requiring adjustments to your diabetes medication. Closely monitor your blood glucose.
- This interaction applies to both insulin and oral antidiabetic drugs. Regular monitoring is crucial.
Potassium-Depleting Diuretics
Some diuretics can lower potassium levels. Prednisone can further deplete potassium, leading to potentially dangerous imbalances. Your doctor may prescribe potassium supplements or adjust your diuretic.
Cardiac Glycosides (e.g., Digoxin)
Prednisone can affect the way your body handles digoxin, a medication for heart conditions. This necessitates careful monitoring of your heart rhythm and digoxin levels.
Other Medications
- Certain antibiotics.
- Some antifungal medications.
- Specific medications for osteoporosis.
These are just a few examples; other interactions are possible. Always consult your healthcare provider to discuss any concerns about potential drug interactions when taking prednisone.
Reporting Adverse Reactions
If you experience any new or worsening symptoms while taking prednisone, particularly a rash or other allergic reaction, promptly contact your doctor. This ensures appropriate management and minimizes potential complications.