Prednisone offers significant relief for polymyalgia rheumatica (PMR) symptoms. Start with a relatively high dose, typically 15-20mg daily, under your doctor’s supervision. This medication quickly reduces inflammation and pain, leading to improved mobility and quality of life. Remember, individual responses vary, so consistent communication with your healthcare provider is key.
Expect to see improvements within days or weeks. However, gradual tapering of the Prednisone dose is crucial to prevent relapse and minimize side effects. Your doctor will create a personalized tapering schedule, carefully reducing your dosage over months. Rapid reduction increases the likelihood of PMR symptoms returning.
Managing side effects is a vital part of Prednisone treatment. Common side effects include weight gain, increased blood sugar, and insomnia. Openly discuss any concerns with your doctor; they can help mitigate these issues through dietary adjustments, medication modifications, or other supportive measures. Regular monitoring of blood pressure and blood sugar is recommended.
While Prednisone is highly effective in managing PMR, it’s not a long-term solution for most. The goal is to achieve remission and then gradually wean off the medication. Alternative treatments, like low-dose methotrexate, may be considered in certain cases, especially for patients experiencing difficulties tapering off Prednisone. Consult your rheumatologist to discuss long-term management strategies.
- Prednisone for Polymyalgia Rheumatica: A Detailed Guide
- Understanding Polymyalgia Rheumatica (PMR)
- Symptoms of PMR
- Diagnosis and Treatment
- Long-Term Management
- Potential Complications
- Prednisone’s Role in PMR Treatment
- Dosage and Administration of Prednisone for PMR
- Initial Dosage and Tapering
- Administration
- Monitoring and Adjustments
- Potential Side Effects
- Important Note:
- Potential Side Effects of Prednisone
- Managing Prednisone Side Effects
- Tapering Off Prednisone: A Gradual Process
- Alternative Treatments and Complementary Therapies
- When to Consult a Doctor Regarding PMR and Prednisone
Prednisone for Polymyalgia Rheumatica: A Detailed Guide
Prednisone rapidly reduces Polymyalgia Rheumatica (PMR) symptoms. Expect significant pain relief within days of starting treatment. Dosage typically begins at 15-20mg daily.
Your doctor will adjust your dosage based on your response. Expect gradual tapering of the dose once symptoms subside, usually over months. Rapid dose reduction can lead to a relapse.
Common side effects include weight gain, fluid retention, increased blood sugar, and mood changes. Maintain a healthy diet and regular exercise to mitigate these. Open communication with your physician is crucial for managing side effects.
Regular blood tests monitor your progress and detect potential complications. These tests help your doctor fine-tune the dosage and duration of your treatment.
Long-term prednisone use carries risks, including osteoporosis and increased risk of infection. Your doctor might prescribe supplemental calcium and vitamin D to protect bone health. Discuss preventative measures against infections with your healthcare provider.
Alternative therapies like physical therapy can complement prednisone treatment, aiding in maintaining mobility and strength during and after treatment.
Remember, prednisone is a powerful medication. Always follow your doctor’s instructions precisely. Report any new or worsening symptoms immediately.
Understanding Polymyalgia Rheumatica (PMR)
Polymyalgia rheumatica (PMR) is an inflammatory condition primarily affecting older adults, usually those over 50. It causes significant muscle pain and stiffness, predominantly in the shoulders and hips. This pain often worsens in the morning and improves with activity.
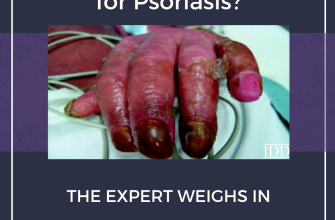
Symptoms of PMR
Recognizing PMR involves understanding its key symptoms: severe aching in the shoulders, neck, hips, and thighs; morning stiffness lasting over an hour; and sometimes, a low-grade fever or fatigue. It’s critical to note that these symptoms can mimic other conditions, so accurate diagnosis is paramount.
Diagnosis and Treatment
Doctors diagnose PMR based on symptoms and blood tests revealing elevated inflammatory markers like ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein). There’s no single definitive test. Prednisone, a corticosteroid, is typically the first-line treatment, effectively reducing inflammation and pain. Careful monitoring of treatment response and potential side effects is needed. Some patients may require other medications along with Prednisone to manage symptoms or side effects. Regular follow-up appointments with your rheumatologist are necessary. The goal is to find the lowest dose of Prednisone that provides adequate relief.
Long-Term Management
Slow tapering of Prednisone is crucial to prevent relapse. Your doctor will gradually reduce your dosage over months or even years. Regular exercise, gentle stretching, and maintaining a healthy weight contribute significantly to long-term management of PMR. Discuss lifestyle modifications with your physician. Early diagnosis and consistent treatment improve outcomes. Contact your doctor immediately if symptoms worsen or new symptoms appear.
Potential Complications
Giant cell arteritis (GCA) is a serious complication associated with PMR. GCA affects the arteries and requires prompt treatment. Symptoms can include headache, jaw claudication (jaw pain with chewing), and vision problems. Report any new or worsening symptoms to your doctor immediately. Early detection and treatment of GCA are critical to prevent vision loss and other severe complications.
Prednisone’s Role in PMR Treatment
Prednisone, a corticosteroid, serves as a cornerstone in Polymyalgia Rheumatica (PMR) treatment. It rapidly reduces inflammation and improves symptoms.
Expect significant pain relief within days of starting treatment. This quick response helps improve mobility and quality of life.
- Dosage: Your doctor will determine the appropriate starting dose, usually high, to quickly control the inflammation. This dose is gradually reduced over months.
- Duration: Treatment typically lasts for at least one year. Premature discontinuation can lead to relapse. Your doctor will monitor your progress and adjust the dosage accordingly.
- Side Effects: While Prednisone is highly effective, potential side effects include weight gain, increased blood sugar, increased blood pressure, and osteoporosis. Open communication with your doctor about any concerns is key.
Weaning off Prednisone requires careful monitoring. A slow, gradual reduction minimizes the risk of relapse and side effects.
- Your doctor will create a personalized tapering schedule.
- Regular blood tests help monitor your progress and adjust the reduction plan.
- Listen to your body. Report any symptoms indicating a relapse immediately.
Beyond Prednisone, lifestyle modifications like regular exercise and a balanced diet can support overall health and well-being during treatment and beyond.
Remember, Prednisone is a powerful medication, and individual responses vary. Regular communication with your rheumatologist ensures optimal management of your PMR.
Dosage and Administration of Prednisone for PMR
Your doctor will determine the correct prednisone dosage based on your individual needs. Typically, treatment begins with a relatively high dose, often 15-20mg daily.
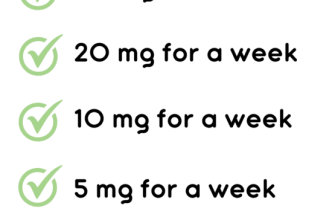
Initial Dosage and Tapering
This higher dose quickly reduces inflammation and improves symptoms. However, long-term high-dose prednisone carries risks. Therefore, your doctor will gradually decrease your dosage over time, a process called tapering. This usually involves reducing the dose by small increments, such as 1-2.5mg every few weeks or months. The tapering schedule is personalized, depending on your response to treatment and the presence of side effects.
- Example Tapering Schedule (Illustrative Only; Always Follow Your Doctor’s Instructions):
- Week 1-4: 20mg daily
- Week 5-8: 17.5mg daily
- Week 9-12: 15mg daily
- …and so on, with continued reductions at your doctor’s discretion.
Administration
Prednisone is usually taken orally, once daily. It’s generally recommended to take it in the morning with food or milk to minimize stomach upset.
Monitoring and Adjustments
Regular check-ups with your doctor are crucial to monitor your progress and adjust the dosage as needed. Blood tests may be used to monitor inflammation markers and assess your overall health.
Potential Side Effects
- Weight gain
- Increased blood sugar
- Mood changes
- Osteoporosis risk increase
- Increased risk of infection
Discuss any side effects you experience with your doctor. They may be able to manage them with medication or lifestyle adjustments. Remember, consistent communication with your healthcare provider is essential throughout the treatment process.
Important Note:
This information is for educational purposes only and should not be considered medical advice. Always consult your physician or rheumatologist for personalized guidance regarding prednisone dosage and treatment for PMR.
Potential Side Effects of Prednisone
Prednisone, while effective for polymyalgia rheumatica, carries potential side effects. Understanding these allows you to work with your doctor to manage them effectively.
Common side effects include weight gain, increased appetite, fluid retention (leading to swelling), and mood changes (such as irritability or anxiety). These often lessen as your dosage decreases.
More serious, though less frequent, side effects need close monitoring. These include:
| Side Effect | Description | Action |
|---|---|---|
| Increased Blood Sugar | Prednisone can elevate blood glucose levels, potentially worsening diabetes. | Regular blood sugar checks are vital. Your doctor may adjust your diabetes medication. |
| Osteoporosis | Long-term prednisone use weakens bones, increasing fracture risk. | Discuss calcium and vitamin D supplements with your physician. Weight-bearing exercise helps. |
| Increased Blood Pressure | Prednisone can raise blood pressure. | Regular blood pressure monitoring and potential adjustments to your blood pressure medication are necessary. |
| Increased Risk of Infection | Prednisone suppresses the immune system, making infections more likely. | Report any signs of infection immediately to your doctor. |
| Cataracts and Glaucoma | Long-term use may increase the risk of eye problems. | Regular eye exams are recommended. |
Always inform your doctor about any new or worsening symptoms. Open communication is key to managing prednisone’s side effects and ensuring your treatment’s success.
Managing Prednisone Side Effects
Monitor your weight regularly. Weight gain is common; adjust your diet accordingly and increase physical activity as tolerated. Consult your doctor about dietary changes.
Pay close attention to your blood pressure. Prednisone can elevate it. Regularly check your blood pressure and discuss any significant changes with your doctor. They might adjust your medication or recommend lifestyle modifications.
Understand the increased risk of infections. Practice good hygiene, avoid crowds during flu season, and contact your doctor immediately if you experience any signs of infection.
Address potential mood swings. Prednisone can affect your mood, causing irritability or anxiety. Openly discuss these changes with your doctor; they may suggest strategies or adjust your medication.
Manage your blood sugar. Prednisone can increase blood sugar levels. Monitor your glucose levels as advised by your doctor and discuss any concerns about managing diabetes or pre-diabetes.
Take measures to protect your bones. Prednisone can increase the risk of osteoporosis. Maintain a calcium-rich diet, consider weight-bearing exercises, and discuss bone density testing with your doctor.
Track and report any gastrointestinal issues. Stomach upset is a possibility. Keep a food diary and discuss any persistent digestive problems with your doctor.
Be aware of potential changes in your skin. Prednisone can thin your skin, increasing your risk of bruising. Use gentle skincare products and report any significant skin changes.
| Side Effect | Management Strategy |
|---|---|
| Increased Appetite | Balanced diet, portion control, increased physical activity |
| Insomnia | Maintain a regular sleep schedule, avoid caffeine before bed |
| Muscle Weakness | Gentle exercise, physical therapy (as advised by your doctor) |
Remember, tapering off prednisone should always be done under your doctor’s supervision. Never stop taking it abruptly. Open communication with your healthcare provider is paramount for effective management of side effects and optimal treatment outcomes.
Tapering Off Prednisone: A Gradual Process
Reduce your Prednisone dose slowly. Your doctor will create a personalized tapering schedule, often decreasing the daily dosage by a small amount, like 1-2.5 mg, every few days or weeks. This gradual reduction minimizes withdrawal symptoms.
Closely monitor your symptoms throughout the tapering process. Report any flare-ups of polymyalgia rheumatica or other concerning symptoms to your physician immediately. They might adjust the tapering schedule to prevent a relapse.
Maintain open communication with your doctor. Regular check-ups allow them to assess your progress and make necessary adjustments to the tapering plan. Don’t hesitate to ask questions; understanding the process empowers you.
Expect some side effects during tapering. Common side effects include fatigue, muscle weakness, and joint pain. These are usually manageable and temporary. Your physician can advise on how to mitigate these.
Consider lifestyle modifications to support your body during tapering. Prioritize sufficient rest, a balanced diet, and regular, gentle exercise as tolerated. These support your body’s natural healing processes.
Once your Prednisone dose is significantly reduced or eliminated, your doctor will likely schedule follow-up appointments to monitor your progress and assess the need for long-term management of polymyalgia rheumatica.
Alternative Treatments and Complementary Therapies
Consider incorporating these approaches alongside Prednisone, always under your doctor’s guidance:
- Low-impact exercise: Gentle activities like swimming or walking can improve flexibility and reduce stiffness. Aim for 30 minutes most days of the week. Consult your physician before starting any new exercise routine.
- Physical therapy: A physical therapist can create a personalized plan including range-of-motion exercises and strengthening techniques, helping manage pain and improve mobility.
- Acupuncture: Some studies suggest acupuncture may offer pain relief for polymyalgia rheumatica. Choose a licensed and experienced practitioner.
Dietary changes may also help:
- Anti-inflammatory diet: Focus on fruits, vegetables, and omega-3 fatty acids found in fish like salmon. Limit processed foods, red meat, and saturated fats.
Other options to explore with your doctor:
- Massage therapy: Gentle massage can help relieve muscle tension and improve circulation.
- Mindfulness and relaxation techniques: Practicing techniques like meditation or deep breathing can help manage stress, which can exacerbate symptoms. Consider yoga or tai chi as well.
Remember, these therapies should complement, not replace, your prescribed medication. Always discuss any alternative treatments with your doctor before starting them to ensure they’re safe and appropriate for your specific situation.
When to Consult a Doctor Regarding PMR and Prednisone
Schedule an appointment immediately if you experience new or worsening symptoms while taking prednisone for polymyalgia rheumatica (PMR). This includes severe muscle weakness, difficulty breathing, vision changes, increased thirst or urination, unexplained weight gain, or significant mood swings.
Contact your doctor if your current PMR symptoms aren’t improving after several weeks of prednisone treatment at the prescribed dosage. Similarly, reach out if your symptoms return after you’ve started tapering your prednisone.
Report any side effects of prednisone, such as increased blood sugar, high blood pressure, easy bruising, or thinning skin. Your doctor can adjust your medication or recommend strategies to manage these side effects.
Regular follow-up appointments are necessary to monitor your PMR and prednisone treatment. These visits allow your doctor to assess your progress, adjust your medication as needed, and address any concerns you may have.
If you have questions or concerns about your prednisone treatment or your PMR symptoms at any time, don’t hesitate to contact your physician. Early intervention can prevent complications and improve your overall health.