Prednisone isn’t an antibiotic; it won’t kill bacteria. Use it only under strict medical supervision for specific situations, like severe inflammatory responses to a bacterial infection, never as a primary treatment. Your doctor might prescribe it to manage symptoms like swelling or inflammation alongside antibiotics.
Common scenarios include severe pneumonia or sepsis where inflammation is causing significant harm. Prednisone reduces inflammation, thereby alleviating some symptoms, potentially improving the patient’s overall condition. However, it’s crucial to understand this doesn’t address the underlying infection itself.
Antibiotics are essential for eliminating the bacteria. Prednisone only acts as an adjunct therapy, managing the body’s overreaction to the infection. Expect your doctor to order regular blood tests and monitor your condition closely while taking both medications. Self-medicating with prednisone is highly dangerous and could worsen your condition.
Potential side effects of prednisone are numerous and can be serious. These include increased blood sugar, weight gain, mood changes, and weakened immunity. Openly discuss any concerns with your physician before starting or continuing treatment to ensure you’re making informed decisions about your health.
- Prednisone for Bacterial Infection: A Detailed Overview
- Situations Where Prednisone Might Be Considered
- Important Considerations and Precautions
- Specific Examples
- Prednisone: Understanding its Role in Inflammation
- Bacterial Infections: Types and Severity
- Factors Influencing Severity
- Recognizing Serious Infections
- Prednisone’s Ineffectiveness Against Bacteria
- Why Prednisone Is Not Used Against Bacterial Infections
- Treating Bacterial Infections: Focus on Antibiotics
- When Prednisone Might Be Used Concurrently with Antibiotics
- Specific Infections and Considerations
- Risks and Monitoring
- Potential Risks of Prednisone Use During Bacterial Infection
- Managing Side Effects of Prednisone
- Consult Your Doctor: The Importance of Professional Guidance
- Why is a Doctor’s Assessment Necessary?
- What to Discuss With Your Doctor
Prednisone for Bacterial Infection: A Detailed Overview
Prednisone is a corticosteroid, not an antibiotic; it doesn’t directly kill bacteria. Therefore, it’s never used alone to treat bacterial infections. Its role is limited to managing inflammation and symptoms associated with a bacterial infection, after the infection has been addressed with antibiotics.
Situations Where Prednisone Might Be Considered
Doctors may prescribe prednisone in conjunction with antibiotics for specific situations. For example, severe bacterial infections like pneumonia sometimes cause significant inflammation in the lungs, leading to respiratory distress. Prednisone can help reduce this inflammation, improving breathing. Similarly, certain severe bacterial infections may trigger overwhelming inflammation throughout the body (septic shock). In these life-threatening situations, prednisone may be used to control this systemic inflammation, supporting the body’s response to antibiotics. However, this is a high-risk situation needing careful medical supervision. The decision to use prednisone is complex and depends on the severity of the infection and the patient’s overall health.
Important Considerations and Precautions
Prednisone carries significant side effects, including increased risk of infection, impaired wound healing, and blood sugar imbalances. Long-term use can lead to more serious complications. Therefore, it’s only used in carefully selected cases, always alongside appropriate antibiotic therapy to combat the underlying infection. Never self-medicate; discuss any potential use of prednisone with your doctor to assess the risks and benefits for your specific situation. They will carefully weigh the potential advantages against the potential harm based on your individual health profile and the nature of the infection.
Specific Examples
Examples of specific bacterial infections where prednisone might be considered alongside antibiotics (under strict medical supervision) include severe cases of bacterial pneumonia or meningitis, alongside antibiotic treatment. This is not an exhaustive list.
This information is for general knowledge and does not constitute medical advice. Consult a healthcare professional for diagnosis and treatment of any medical condition.
Prednisone: Understanding its Role in Inflammation
Prednisone doesn’t treat bacterial infections directly; it targets inflammation. This is a key distinction.
Inflammation is your body’s response to injury or infection. It involves:
- Swelling
- Pain
- Redness
- Heat
- Loss of function
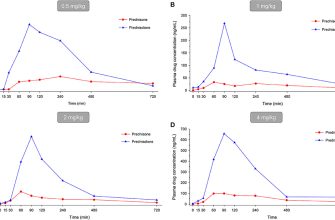
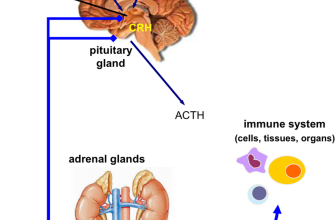
Prednisone, a corticosteroid, reduces these symptoms by suppressing the immune system’s inflammatory response. It does this by decreasing the production of inflammatory chemicals.
Specifically, Prednisone influences several key processes:
- Reduces the number of immune cells (like white blood cells) at the site of inflammation.
- Decreases the production of inflammatory cytokines (signaling molecules).
- Stabilizes cell membranes, reducing damage.
However, remember: Prednisone doesn’t kill bacteria. Antibiotics are necessary to treat a bacterial infection. Doctors might prescribe Prednisone alongside antibiotics to manage the inflammation caused by the infection, improving patient comfort and potentially speeding recovery from associated symptoms. This combined approach requires careful medical supervision due to potential side effects of both Prednisone and antibiotics.
Always consult a physician for guidance on medication use. They will assess your individual needs and determine the most appropriate treatment plan. Self-treating can be harmful.
Bacterial Infections: Types and Severity
Bacterial infections manifest in diverse ways, depending on the bacteria involved and the body’s response. Common examples include strep throat (caused by Streptococcus pyogenes), pneumonia (often caused by Streptococcus pneumoniae or Haemophilus influenzae), urinary tract infections (UTIs, frequently caused by Escherichia coli), and skin infections (like impetigo, caused by Staphylococcus aureus or Streptococcus pyogenes). The severity ranges from mild to life-threatening.
Factors Influencing Severity
Several factors influence the severity of a bacterial infection. The virulence of the bacteria–their ability to cause disease–plays a crucial role. A highly virulent strain will likely cause a more severe infection. The location of the infection matters; infections in critical areas like the bloodstream (sepsis) or meninges (meningitis) are far more dangerous than a localized skin infection. The patient’s immune system also heavily influences the outcome; a weakened immune system allows infections to progress more rapidly and severely.
Recognizing Serious Infections
Signs of a serious bacterial infection can include high fever, persistent chills, severe pain, difficulty breathing, rapid heart rate, confusion, and decreased urination. Seek immediate medical attention if you experience these symptoms. Delaying treatment can lead to serious complications, including organ damage and death. Early diagnosis and appropriate antibiotic treatment are vital for a favorable outcome.
Prednisone’s Ineffectiveness Against Bacteria
Prednisone won’t kill bacteria. It’s a corticosteroid, reducing inflammation, not a bactericide or antibiotic. Therefore, it’s ineffective as a standalone treatment for bacterial infections.
Why Prednisone Is Not Used Against Bacterial Infections
Prednisone’s mechanism of action focuses on suppressing the body’s immune response. While this can be beneficial in certain situations (like autoimmune diseases), it can also hinder the body’s ability to fight bacterial infections. Suppressed immunity allows bacterial growth, potentially worsening the infection.
Treating Bacterial Infections: Focus on Antibiotics
Antibiotics directly target and destroy bacteria. If you suspect a bacterial infection, seek medical attention. A doctor will diagnose the infection and prescribe the appropriate antibiotic. Never self-treat bacterial infections. Incorrect treatment can lead to antibiotic resistance and prolonged illness.
Remember: Prednisone might be prescribed alongside antibiotics to manage inflammation resulting from a bacterial infection, but it never replaces antibiotic treatment.
When Prednisone Might Be Used Concurrently with Antibiotics
Prednisone, a corticosteroid, is sometimes used alongside antibiotics, but only under strict medical supervision. This is not a standard practice and should never be self-initiated.
One scenario is severe bacterial infections causing overwhelming inflammation. For example, in cases of bacterial meningitis or severe pneumonia, high doses of antibiotics are often paired with prednisone to quickly reduce inflammation and potentially improve patient outcomes. The prednisone helps control the body’s inflammatory response, which can itself cause significant damage.
Specific Infections and Considerations
While there is no blanket approval, certain infections might warrant this combined approach, though research remains ongoing. Always discuss this with your doctor. Individual responses vary greatly.
| Infection Type | Possible Reason for Concomitant Prednisone Use | Important Note |
|---|---|---|
| Tuberculosis (TB) | Reduce inflammation in severe cases, particularly during the early stages of treatment. | Prednisone is only used under strict guidelines and with rigorous monitoring due to the immunosuppressive effects. |
| Sepsis (severe blood infection) | Dampen the “cytokine storm” that can occur, potentially reducing organ damage. | This is a high-risk scenario demanding specialized medical expertise. |
Risks and Monitoring
Combining prednisone and antibiotics increases the risk of side effects, including increased susceptibility to other infections and impaired wound healing. Regular monitoring of blood counts, organ function, and blood sugar levels is necessary. Your doctor will carefully weigh the potential benefits against these risks.
Potential Risks of Prednisone Use During Bacterial Infection
Prednisone, while effective for inflammation, weakens your immune system, hindering your body’s fight against bacteria. This increased susceptibility makes infections worse and potentially life-threatening.
Specifically, prednisone can mask symptoms of infection, delaying diagnosis and treatment. A seemingly improving condition could actually be a worsening infection hidden by the prednisone’s anti-inflammatory effects. This delayed treatment can lead to serious complications like sepsis or organ damage.
Moreover, prednisone increases the risk of developing secondary infections, particularly fungal infections. Your weakened immune system struggles to combat new invaders that might not pose a threat under normal circumstances.
Studies show a correlation between prednisone use and prolonged recovery times from bacterial infections. The body’s natural healing process is hampered, resulting in extended illness and a greater need for antibiotics.
Finally, certain bacterial infections respond poorly to prednisone alongside antibiotics. The drug’s impact on the immune response may interfere with the antibiotic’s efficacy, compromising the overall treatment strategy. Always consult a doctor to determine if prednisone is appropriate for your specific case.
Managing Side Effects of Prednisone
Prednisone, while effective in treating inflammation, can cause several side effects. Monitor for increased thirst and frequent urination, indicative of high blood sugar. Maintain a balanced diet and check your blood sugar regularly if you have diabetes or risk factors.
Weight gain is common. Focus on a healthy diet and regular exercise to mitigate this. Consult your doctor about diet and exercise plans suitable for you.
Mood changes, like irritability or anxiety, are possible. Maintain open communication with your doctor and loved ones. Consider stress-reducing techniques such as meditation or yoga.
Prednisone weakens the immune system, increasing infection risk. Practice good hygiene and avoid contact with sick individuals. Report any signs of infection immediately to your doctor.
High blood pressure is another potential side effect. Regular blood pressure monitoring is crucial. Your doctor may adjust your medication or recommend lifestyle changes.
Muscle weakness and bone thinning can occur with prolonged use. Engage in weight-bearing exercise under your doctor’s guidance. A balanced diet rich in calcium and vitamin D is also helpful.
Insomnia is frequently reported. Maintain a regular sleep schedule, create a relaxing bedtime routine, and limit caffeine and alcohol intake before bed. If problems persist, discuss sleep aids with your doctor.
Remember to inform your doctor about any side effects you experience. They can help you manage these effects and adjust your treatment plan accordingly.
Consult Your Doctor: The Importance of Professional Guidance
Prednisone is a powerful medication, and using it incorrectly can worsen a bacterial infection or cause harmful side effects. Never self-treat a bacterial infection with prednisone.
Always seek medical advice before starting any new medication, especially for treating infections. A doctor will perform a thorough examination, identify the specific bacteria causing the infection, and determine the appropriate treatment plan. This includes considering your medical history, allergies, and other medications you are currently taking.
Why is a Doctor’s Assessment Necessary?
- Accurate Diagnosis: Doctors use lab tests (like blood cultures and sensitivity testing) to precisely identify the bacteria, confirming the infection and its severity. This ensures the right antibiotic is prescribed.
- Appropriate Treatment: Prednisone might be part of a broader treatment strategy, used alongside antibiotics to manage inflammation. A doctor designs the plan tailored to your needs, considering potential drug interactions.
- Monitoring Side Effects: Prednisone has potential side effects, ranging from mild to severe. A doctor monitors you closely for any adverse reactions, making necessary adjustments to dosage or treatment.
- Personalized Approach: Your health history and current condition significantly influence treatment decisions. A personalized approach ensures optimal outcomes and minimal risks.
What to Discuss With Your Doctor
- Your symptoms, including when they started and their severity.
- Your complete medical history, including allergies and current medications.
- Any pre-existing health conditions.
- Your lifestyle factors (diet, exercise, smoking).
- Your expectations and concerns regarding treatment.
Prompt medical attention is key to successful infection management and minimizing health risks. Don’t delay – contact your doctor immediately if you suspect a bacterial infection.