Prednisone, a powerful corticosteroid, carries a risk of avascular necrosis (AVN), a serious condition where bone tissue dies due to lack of blood supply. This risk increases with higher doses and longer treatment durations. Regular monitoring is key.
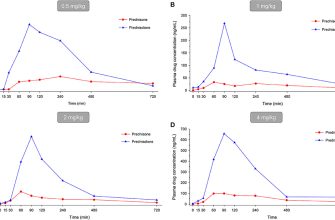
Specifically, studies show a correlation between cumulative prednisone dosage exceeding 40 mg daily for over three months and a significantly elevated AVN risk. Patients should discuss this risk with their doctors to weigh the benefits of prednisone against potential bone complications. Early detection is crucial for effective management.
Regular bone density scans can help detect early signs of AVN. Your doctor might recommend lifestyle modifications, like weight management, to reduce stress on your joints. In some cases, bisphosphonates or other medications might be prescribed to help maintain bone health. Open communication with your healthcare provider is paramount.
Remember: This information is for educational purposes and does not substitute professional medical advice. Consult your physician or rheumatologist for personalized assessment and treatment strategies related to your prednisone use and potential AVN risk.
- Prednisone and Avascular Necrosis: A Detailed Look
- Understanding Avascular Necrosis (AVN)
- Prednisone’s Role in AVN Development
- Understanding the Mechanism
- Minimizing Your Risk
- Specific Considerations
- Risk Factors Beyond Prednisone Use
- Recognizing the Symptoms of AVN
- Changes in Joint Movement
- Other Possible Symptoms
- Diagnosis and Imaging Techniques for AVN
- Initial Imaging Modalities
- Advanced Imaging Techniques
- Interpreting Results
- Treatment Options for Prednisone-Induced AVN
- Prevention Strategies and Lifestyle Changes
Prednisone and Avascular Necrosis: A Detailed Look
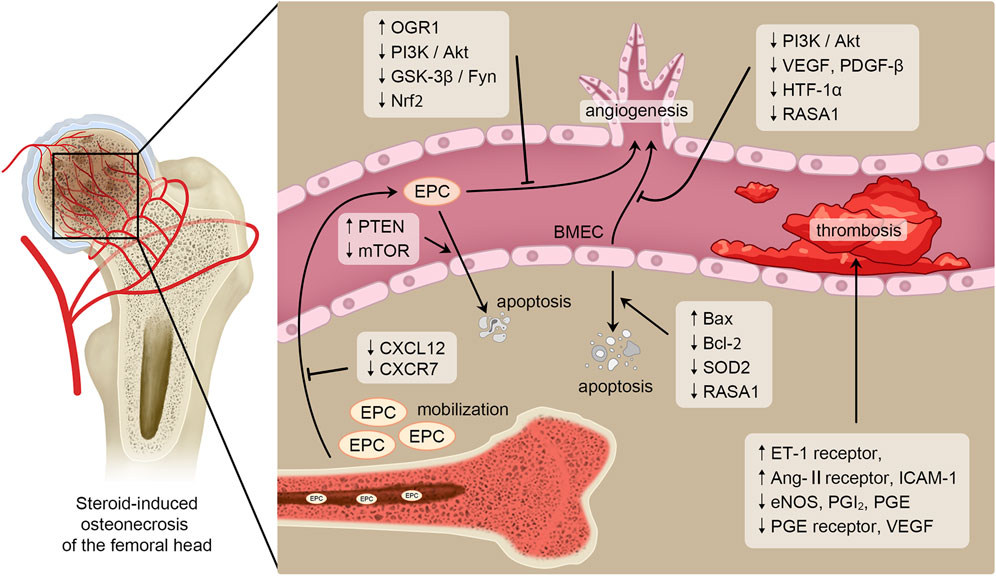
High-dose prednisone use significantly increases your risk of avascular necrosis (AVN), also known as osteonecrosis. This occurs because prednisone disrupts blood flow to the bone, leading to bone death. The risk is dose-dependent: higher doses and longer treatment durations pose a greater threat.
Commonly affected joints include the hip, knee, and shoulder. Symptoms often begin subtly, with pain worsening gradually. Early diagnosis is critical, as early intervention can improve outcomes. Your doctor will likely use imaging techniques like X-rays or MRI scans to confirm a diagnosis.
Risk factors beyond prednisone include alcohol abuse, sickle cell disease, and certain types of trauma. These factors, when combined with prednisone use, dramatically increase your AVN risk.
Treatment options vary depending on the severity and location of the AVN. Non-surgical approaches such as pain management medication, physical therapy, and bisphosphonates may be sufficient for some. However, more severe cases may necessitate surgery, potentially involving bone grafting or joint replacement.
Regular monitoring is crucial, especially during and after prednisone treatment. This includes bone density scans and regular check-ups to assess for any signs or symptoms of AVN. Open communication with your doctor is key; report any new joint pain or stiffness immediately.
While prednisone is a powerful medication with many benefits, understanding and mitigating the risk of AVN is paramount. Discuss all potential risks and benefits with your physician before starting or continuing prednisone treatment. They can help you weigh the medication’s benefits against the individual risk of developing AVN.
Understanding Avascular Necrosis (AVN)
Avascular necrosis (AVN), also known as osteonecrosis, occurs when blood supply to a bone is interrupted. This lack of blood flow leads to bone death. The hip joint is most commonly affected, but AVN can also impact other joints like the shoulders, knees, and ankles.
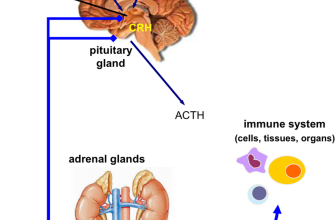
Several factors contribute to AVN. Long-term corticosteroid use, like Prednisone, is a significant risk factor. Other causes include fractures, radiation therapy, sickle cell disease, and excessive alcohol consumption. The precise mechanism varies depending on the underlying cause, but the result is always the same: bone tissue dies.
Symptoms often start subtly. You might initially experience mild pain, particularly with weight-bearing activities. As the condition progresses, pain becomes more intense and persistent, even at rest. Joint stiffness and limited range of motion are also common. In advanced cases, the bone may collapse, causing deformity and severe disability.
Diagnosis typically involves physical examination, X-rays, and potentially MRI scans for early detection. Early diagnosis is critical for effective treatment. Treatment options depend on the severity and location of the AVN. They range from conservative measures like pain management and physical therapy to surgical interventions such as bone grafts or joint replacement.
Managing AVN often requires a multidisciplinary approach involving orthopedic surgeons, pain specialists, and physical therapists. A proactive approach, including regular monitoring and prompt treatment, significantly improves outcomes. Lifestyle modifications, such as weight management and avoiding high-impact activities, can also help.
Prednisone’s Role in AVN Development
Prednisone, a potent corticosteroid, significantly increases your risk of avascular necrosis (AVN). This happens because it disrupts blood flow to your bones. The higher the dose and the longer you take it, the greater your risk becomes. Studies show a clear correlation: prolonged prednisone use of over 3 months at high doses (over 20mg per day) presents a substantially elevated risk.
Understanding the Mechanism
Prednisone affects bone cells, reducing the production of collagen and other crucial proteins. This weakens the bone structure, leaving it more vulnerable to damage and, critically, impairing its ability to heal efficiently from minor injuries, increasing the likelihood of AVN development.
Minimizing Your Risk
Early detection is key. Regular bone density scans, especially if you are on long-term prednisone therapy, can help detect early signs of AVN. Maintain a healthy lifestyle. This includes a balanced diet rich in calcium and vitamin D, regular weight-bearing exercise (to promote bone health), and avoiding smoking (which further compromises blood flow). Collaborate closely with your doctor. Discuss your individual risk factors and treatment options. They might consider alternative medications, lower prednisone dosages, or bone-protecting medications.
Specific Considerations
Genetic predisposition plays a role. Family history of AVN increases individual susceptibility. Other medications you’re taking can influence your risk; inform your doctor about all your medications and supplements. Underlying health conditions such as autoimmune diseases can amplify AVN risk.
Risk Factors Beyond Prednisone Use
Beyond prednisone, several factors significantly increase your risk of avascular necrosis (AVN). High alcohol consumption damages blood vessels, reducing blood flow to the bone and increasing AVN risk. Similarly, smoking constricts blood vessels, creating a similar negative impact.
Certain medical conditions predispose individuals to AVN. Sickle cell disease, a blood disorder, causes abnormal blood cells to block blood flow, increasing AVN likelihood. Gaucher’s disease, a genetic disorder affecting fat metabolism, also elevates AVN risk.
Joint injuries, such as hip dislocations or fractures, can disrupt blood supply to the bone, leading to AVN. This damage often requires prompt medical attention.
Radiation therapy, while effective in cancer treatment, can harm blood vessels in bones, increasing the chance of AVN. This risk should be discussed thoroughly with your oncologist.
Obesity places added stress on weight-bearing joints, potentially contributing to reduced blood flow and consequently, increasing AVN risk. Maintaining a healthy weight is crucial.
Some medications, beyond corticosteroids, can also increase your AVN risk. Discuss any medication you are taking with your doctor to assess potential interactions.
Age is also a factor; older individuals tend to have reduced blood flow to their bones, increasing susceptibility to AVN. This is a natural process that’s difficult to control.
Recognizing the Symptoms of AVN
Pay close attention to any pain in your hip, shoulder, knee, or wrist. This pain often begins gradually and worsens over time. It might feel deep within the joint and radiate to surrounding areas. Initially, it may only appear during activity, but as AVN progresses, you might experience pain even at rest.
Changes in Joint Movement
Reduced range of motion is a common indicator. You may find it increasingly difficult to bend, straighten, or rotate the affected joint. Stiffness and a feeling of locking or catching are also possible. These limitations can significantly impact your daily activities.
Other Possible Symptoms
Depending on the severity and location of the AVN, you might also experience swelling, tenderness to the touch around the affected joint, muscle weakness, or a limping gait. In advanced cases, the joint may collapse, causing noticeable deformity and significant pain.
If you suspect you have AVN, consult a doctor immediately. Early diagnosis is critical for effective treatment.
Diagnosis and Imaging Techniques for AVN
Early detection is key to managing avascular necrosis (AVN). Doctors rely heavily on imaging studies to confirm a diagnosis.
Initial Imaging Modalities
- X-rays: These are often the first imaging test. While they might not show early AVN changes, later-stage AVN presents as bone collapse or sclerosis. Expect to see crescent signs or subchondral lucency.
- MRI: Magnetic resonance imaging offers superior sensitivity in detecting early AVN. It clearly visualizes bone marrow edema, even before x-ray changes are apparent. MRI remains the gold standard for early detection.
If MRI confirms AVN, further imaging may be necessary to assess the extent and severity of the necrosis.
Advanced Imaging Techniques
- Bone Scan: This nuclear medicine technique can detect AVN in its earlier stages than plain x-rays. It shows increased uptake in the affected area indicating the presence of inflammation and bone remodeling.
- CT Scan: Computed tomography provides detailed cross-sectional images, useful for assessing bone structure and the presence of fractures or other associated abnormalities. CT scans are particularly helpful in assessing the extent of bone involvement.
The choice of imaging modality depends on factors such as clinical presentation, disease stage, and the availability of resources. Your physician will determine the most appropriate imaging approach for your specific situation. Remember, early and accurate diagnosis directly impacts treatment outcomes and helps determine the best course of action.
Interpreting Results
Radiologists interpret imaging results, providing detailed reports for your physician. These reports describe the location, size, and severity of the AVN, aiding in treatment planning. Always discuss your results with your doctor to understand their implications for your treatment.
Treatment Options for Prednisone-Induced AVN
Managing prednisone-induced avascular necrosis (AVN) focuses on slowing disease progression and relieving symptoms. Treatment depends on the severity and location of the AVN.
For early-stage AVN, conservative management is often the first approach. This includes:
- Pain management: Over-the-counter pain relievers like ibuprofen or naproxen, or prescription medications if needed.
- Activity modification: Reducing weight-bearing activities on the affected joint to minimize stress.
- Bisphosphonates: These medications can improve bone density and may slow AVN progression. Your doctor will determine suitability.
If conservative treatment fails to control pain or the AVN progresses, surgical intervention may be necessary. Options include:
| Surgical Procedure | Description |
|---|---|
| Core decompression | Drilling holes in the affected bone to relieve pressure and improve blood flow. |
| Bone grafting | Replacing damaged bone tissue with healthy bone from another area of the body or a bone graft substitute. |
| Joint replacement | Replacing the severely damaged joint with a prosthetic implant. This is typically a last resort for advanced cases. |
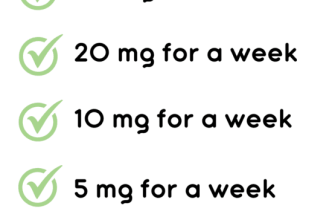
Reducing prednisone dosage, when feasible, is also vital. Your doctor will carefully manage any prednisone tapering to minimize potential complications.
Regular monitoring through imaging studies (X-rays, MRI) is crucial to track disease progression and assess the effectiveness of treatment. Close collaboration with your physician is paramount for optimal management of your condition.
Prevention Strategies and Lifestyle Changes
Maintain a healthy weight. Excess weight puts extra stress on your joints, increasing the risk of avascular necrosis (AVN). Aim for a Body Mass Index (BMI) within the healthy range.
Protect your joints. Avoid high-impact activities like running or jumping that can further damage your bones. Consider low-impact exercises such as swimming or cycling.
Strengthen your bones. Weight-bearing exercises, such as walking and strength training, improve bone density and reduce the risk of fractures.
- Engage in regular strength training, focusing on major muscle groups at least twice a week.
- Incorporate at least 30 minutes of moderate-intensity aerobic exercise most days of the week.
Improve your diet. Consume a balanced diet rich in calcium and vitamin D. Calcium is crucial for strong bones, and vitamin D aids calcium absorption.
- Include calcium-rich foods like dairy products, leafy greens, and fortified foods in your diet.
- Ensure adequate Vitamin D intake through sunlight exposure (safely), or supplements if necessary.
Quit smoking. Smoking significantly restricts blood flow, increasing the risk of AVN. Stopping smoking is a vital step in protecting your bone health.
Limit alcohol consumption. Excessive alcohol intake can also impair blood flow and negatively impact bone health.
Monitor your Prednisone dosage. Work closely with your doctor to manage your Prednisone prescription and minimize long-term use if possible. Regular blood tests help monitor for any side effects.
- Attend all scheduled appointments with your physician.
- Report any new or worsening symptoms immediately.
Consult with your doctor about bisphosphonates. These medications can help strengthen bones and reduce the risk of fractures, particularly if you’re at high risk for AVN.