Prednisone can significantly reduce allergy symptoms, acting quickly to quell inflammation. It’s a powerful corticosteroid, however, so understanding its uses and potential side effects is paramount before use. Your doctor should always guide your treatment plan.
Specifically, prednisone works by suppressing the immune system’s response to allergens. This translates to less swelling, itching, and inflammation associated with allergic reactions like hay fever, hives, or eczema. Remember, it treats symptoms, not the underlying allergy itself.
While effective, prednisone is not a long-term solution for allergies. Prolonged use carries risks, including increased susceptibility to infections, weight gain, and changes in mood. Your doctor will likely prescribe a short course, or use it strategically for severe flare-ups.
Always discuss prednisone with your doctor before starting any treatment. They can assess your specific allergy, health conditions, and prescribe the most appropriate dosage and duration. This ensures safe and effective management of your allergy symptoms.
Alternative treatment options, such as antihistamines or immunotherapy, should be considered as part of a comprehensive allergy management plan. These may provide long-term relief without the side effects associated with prednisone.
- Prednisone and Allergies: A Detailed Guide
- Prednisone’s Role in Treating Allergic Reactions
- Potential Side Effects and Risks of Prednisone Use for Allergies
- Common Side Effects
- Less Common but Serious Side Effects
- When to Consider Prednisone and Alternatives for Allergy Management
- Alternatives to Prednisone
- Understanding Side Effects
Prednisone and Allergies: A Detailed Guide
Prednisone, a corticosteroid, powerfully suppresses the immune system, offering significant allergy relief. It effectively reduces inflammation, a key component of allergic reactions. This means it can quickly alleviate symptoms like sneezing, itching, and swelling.
However, prednisone isn’t a long-term solution for allergies. Its potent effects come with potential side effects, including weight gain, increased blood sugar, and increased risk of infection. Doctors typically prescribe it for short, intense allergy flare-ups rather than ongoing management.
Always follow your doctor’s instructions precisely regarding dosage and duration. Never alter your dosage without consulting your physician. They will help determine the appropriate dosage based on your specific needs and allergy severity.
Commonly, prednisone is used to manage severe allergic reactions like anaphylaxis, where immediate and potent anti-inflammatory action is required. It also finds application in treating severe allergic asthma or allergic rhinitis. For less severe allergies, other treatments, such as antihistamines or immunotherapy, are often preferred due to the potential side effects of prednisone.
Be aware of potential side effects and promptly report any unusual symptoms to your doctor. These could include mood changes, insomnia, or gastrointestinal issues. Your doctor can monitor you and adjust treatment accordingly.
While prednisone can be highly effective in controlling allergy symptoms quickly, a long-term allergy management plan usually involves a combination of other approaches. This might include allergy testing to pinpoint specific triggers, allergen avoidance, and regular medication to manage symptoms. Discuss a long-term strategy with your allergist or physician.
Prednisone’s Role in Treating Allergic Reactions
Prednisone, a corticosteroid, powerfully reduces inflammation. This makes it highly effective in managing severe allergic reactions.
It works by decreasing the activity of your immune system, thereby lessening the body’s response to allergens. This translates to reduced swelling, itching, and other symptoms.
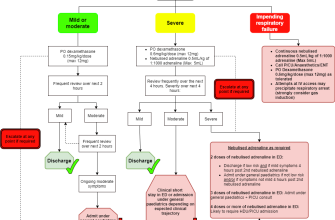
- For severe allergic reactions like anaphylaxis: Prednisone provides rapid relief, often administered alongside other treatments like epinephrine.
- For less severe allergic reactions: It can effectively control symptoms like hives, swelling, and breathing difficulties, reducing the need for other medications.
- For allergic reactions involving the lungs (e.g., asthma exacerbation due to allergens): Prednisone quickly reduces airway inflammation and improves breathing.
Prednisone is typically a short-term treatment for allergic reactions. Long-term use carries potential side effects, so your doctor will carefully monitor your condition and adjust the dosage accordingly.
- Your doctor will determine the appropriate dosage based on the severity of your reaction and your overall health.
- They will likely prescribe a tapering schedule to gradually reduce the dose to minimize side effects.
- Be sure to discuss any potential side effects, such as increased appetite, insomnia, or mood changes, with your doctor.
Remember, Prednisone treats the symptoms of an allergic reaction but doesn’t address the underlying cause. Allergy testing and immunotherapy may be necessary for long-term management.
Potential Side Effects and Risks of Prednisone Use for Allergies
Prednisone, while effective for allergy symptom relief, carries potential side effects. These vary depending on dosage and duration of treatment. Higher doses and longer treatment periods increase the risk of experiencing more side effects.
Common Side Effects
Common side effects include increased appetite and weight gain, fluid retention (causing swelling), mood changes (like irritability or anxiety), insomnia, and increased blood sugar. Some individuals experience indigestion or heartburn. These usually lessen or disappear once you stop taking Prednisone.
Less Common but Serious Side Effects
Less frequent but more serious potential side effects include increased risk of infection due to immunosuppression, thinning of the bones (osteoporosis), high blood pressure, cataracts, and glaucoma. Rarely, Prednisone can trigger more serious complications like muscle weakness, pancreatitis, and psychological issues. These are more likely with prolonged high-dose use.
Regular monitoring by your doctor is crucial, especially if you are on Prednisone for an extended period. They can track your progress, adjust dosage as needed, and address any concerns. Openly discussing any side effects you experience with your physician is paramount for safe and effective management.
Remember to never stop taking Prednisone abruptly without consulting your doctor. Dosage reduction must be gradual to avoid withdrawal symptoms. Your doctor will help you create a safe tapering schedule.
When to Consider Prednisone and Alternatives for Allergy Management
Prednisone, a corticosteroid, powerfully reduces inflammation, making it effective for severe allergic reactions like anaphylaxis or severe asthma exacerbations requiring immediate relief. Doctors prescribe it for short-term use only, due to potential side effects. Consider prednisone when other treatments fail to control symptoms, or for a rapid response to a severe allergic event.
Alternatives to Prednisone
Many effective allergy management strategies exist. First-line treatment often includes antihistamines (like cetirizine or fexofenadine) for milder symptoms. For moderate to severe allergies, leukotriene modifiers (like montelukast) or nasal corticosteroids (like fluticasone) may be prescribed. Immunotherapy, also known as allergy shots, offers long-term symptom relief by gradually desensitizing the body to allergens. Always discuss treatment options with your doctor to determine the best approach for your specific needs and allergies. Specific immunotherapy requires a commitment of several months or years, while other treatments can provide faster relief.
Understanding Side Effects
Prednisone’s side effects can include weight gain, increased blood sugar, mood changes, and weakened immune system. Your doctor will carefully weigh the benefits against these risks. Alternatives, while potentially less powerful in acute situations, generally carry fewer significant side effects. Discuss all potential benefits and drawbacks with your physician before starting any treatment.