Seek immediate medical attention if you’re considering or receiving a 1000mg IV Prednisone dose. This high dosage demands close monitoring by a healthcare professional due to the significant risk of side effects.
High-dose Prednisone (like 1000mg IV) is typically reserved for severe conditions, such as severe allergic reactions, or life-threatening inflammatory disorders. Your doctor will carefully weigh the benefits against potential risks before prescribing this treatment.
Expect rigorous monitoring. Your physician will likely order frequent blood tests to assess your blood sugar, electrolytes, and other vital indicators. They will also monitor for potential complications such as fluid retention, infections, and changes in blood pressure. Regular follow-up appointments are critical.
Medication adherence is paramount. Strictly follow your doctor’s instructions regarding administration, dosage, and duration of treatment. Report any unusual symptoms immediately. This includes, but isn’t limited to, severe headaches, blurred vision, rapid heartbeat, or significant changes in mood.
Remember, this information serves as a concise overview and should not replace professional medical advice. Always consult your healthcare provider for personalized guidance and treatment tailored to your specific condition.
- Prednisone 1000 mg IV: A Detailed Overview
- What is Prednisone and its IV Administration?
- Therapeutic Uses of High-Dose Prednisone (1000mg IV)?
- Autoimmune Diseases
- Other Conditions
- Important Considerations
- Administration Protocol and Dosage Considerations
- Potential Side Effects and Complications
- Monitoring and Management of Adverse Reactions
- Patient Education and Support
- Managing Side Effects
- Medication and Follow-up
- Interactions with Other Medications
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Blood Thinners
- Diabetes Medications
- Potassium-Depleting Diuretics
- Immunosuppressants
- Long-Term Implications and Tapering Strategies
Prednisone 1000 mg IV: A Detailed Overview
Prednisone 1000 mg IV is a high dose, typically administered for severe inflammatory conditions. This dosage requires close medical supervision due to potential side effects.
Administration usually involves a slow intravenous infusion over at least 30 minutes to minimize the risk of adverse reactions. Rapid infusion can cause significant cardiovascular events.
Common side effects include increased blood sugar, fluid retention, hypertension, and mood changes. Patients should monitor their blood pressure and blood glucose regularly. Serious side effects are rare but include infections, gastrointestinal bleeding, and pancreatitis. Report any unusual symptoms to your doctor immediately.
This high dose is not usually sustained for prolonged periods. The duration of treatment depends entirely on the underlying condition and clinical response. Tapering of the dose is essential to avoid adrenal insufficiency.
Before treatment, your doctor will assess your current health status, including existing conditions and medications. This assessment helps determine the suitability of Prednisone 1000 mg IV and allows for appropriate monitoring during therapy.
Regular blood tests might be necessary to monitor blood counts, liver function, and electrolyte levels. These tests help detect any potential complications early and allow for timely intervention.
This information is for educational purposes only and does not substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
What is Prednisone and its IV Administration?
Prednisone is a corticosteroid medication, a synthetic version of the hormone cortisol. Doctors prescribe it to reduce inflammation and suppress the immune system. IV administration delivers prednisone directly into the bloodstream, ensuring rapid absorption and higher initial concentrations compared to oral forms.
Uses: Prednisone IV is used to treat various conditions requiring rapid and potent anti-inflammatory or immunosuppressive effects. These include severe allergic reactions, autoimmune diseases (like lupus), certain cancers, and acute exacerbations of chronic inflammatory conditions.
Important Note: High-dose IV prednisone, like 1000 mg, is usually reserved for severe cases and requires careful monitoring by a medical professional due to potential side effects.
Administration: A healthcare professional administers the IV infusion, typically over a specific time period (e.g., 30 minutes to several hours) to minimize adverse reactions. The dosage and infusion rate depend on the individual’s condition and response to treatment.
Side Effects: Possible side effects include increased blood sugar, fluid retention, mood changes, increased risk of infections, and gastrointestinal issues. Your doctor will discuss potential risks and benefits before initiating treatment.
Monitoring: Regular blood tests and monitoring of vital signs are essential during and after IV prednisone administration to detect and manage potential complications. Your physician will outline a suitable monitoring schedule based on your specific needs.
Dosage Adjustments: The prednisone dose may be adjusted based on the patient’s response to treatment and any potential side effects. Never adjust the dosage without consulting with a doctor.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Therapeutic Uses of High-Dose Prednisone (1000mg IV)?
High-dose intravenous Prednisone (1000mg) is reserved for severe, life-threatening conditions. Its primary applications involve rapid, intense immunosuppression. This makes it useful in managing severe autoimmune diseases experiencing an acute exacerbation, such as:
Autoimmune Diseases
Severe cases of lupus, including lupus nephritis, and rapidly progressive glomerulonephritis often benefit from this aggressive approach. Similarly, severe rheumatoid arthritis flares, particularly those affecting multiple organ systems, may warrant high-dose Prednisone. We also see its use in certain types of vasculitis, especially those threatening vital organs.
Other Conditions
High-dose Prednisone also plays a role in managing severe allergic reactions, such as anaphylaxis, and certain types of acute organ rejection following transplantation. It’s crucial to remember this is a last resort, used only when other treatments have proven insufficient, due to the significant side effects associated with such high doses. Always consult medical guidelines and relevant literature for the most up-to-date treatment protocols.
Important Considerations
High-dose Prednisone requires close monitoring for complications, including hyperglycemia, infections, fluid retention, and psychological effects. The duration of treatment should be as short as possible, and tapering schedules are crucial to prevent rebound effects. Individual patient responses vary, making careful assessment and adjustment of therapy vital.
Administration Protocol and Dosage Considerations
Prednisone 1000 mg IV should be administered by a qualified healthcare professional in a controlled medical setting. Direct intravenous injection is the recommended route. Rapid administration may lead to hypotension, so a slow infusion over at least 30 minutes is generally preferred.
Dosage adjustments: The 1000 mg dose is typically used for severe inflammatory conditions and requires close monitoring. Patients with renal or hepatic impairment may necessitate reduced dosages. Adjustments are based on individual patient response and clinical status, guided by blood tests and vital signs. Frequent monitoring of blood glucose levels is crucial, especially in patients with diabetes or a predisposition to hyperglycemia.
Specific guidance: Always refer to current clinical guidelines and individual patient medical history. Consider co-existing conditions and potential drug interactions. The prescribing physician should provide tailored instructions based on the patient’s unique circumstances.
Monitoring: Regular assessment of blood pressure, heart rate, and electrolytes is required during and after administration. Close observation for signs of infection, fluid retention, and gastrointestinal distress is essential. Patients should be educated on potential side effects and advised to report any unusual symptoms immediately.
Contraindications: Prednisone should not be administered to patients with known hypersensitivity to corticosteroids. Use caution in individuals with systemic fungal infections, severe hypertension, or active peptic ulcers.
Potential Side Effects and Complications
A high-dose Prednisone IV infusion like 1000mg carries significant risks. Understanding these potential side effects is crucial for informed decision-making and prompt management.
Immediate Reactions: You might experience allergic reactions, including hives, swelling, or difficulty breathing. Seek immediate medical attention if this occurs.
- Increased Blood Sugar: Prednisone elevates blood glucose levels. Regular blood sugar monitoring is necessary, especially for individuals with diabetes.
- Fluid Retention: Expect potential swelling in your legs, ankles, and face due to fluid retention. Limit sodium intake.
- Increased Blood Pressure: Your blood pressure may rise. Regular monitoring and adjustments to medication may be needed.
Longer-Term Effects: Prolonged high-dose Prednisone use can lead to several complications:
- Osteoporosis: Prednisone weakens bones, increasing fracture risk. Calcium and vitamin D supplementation, along with weight-bearing exercise, are recommended.
- Muscle Weakness: This is a common side effect, potentially leading to difficulties with mobility. Gentle exercise, as advised by your doctor, may help.
- Infections: Prednisone suppresses the immune system, raising your vulnerability to infections. Report any signs of infection immediately.
- Mood Changes: Irritability, anxiety, and depression can occur. Discuss any mental health changes with your physician.
- Gastrointestinal Issues: Prednisone can cause heartburn, ulcers, and pancreatitis. Report any stomach pain or discomfort.
- Cataracts and Glaucoma: Long-term use increases the risk of eye problems. Regular eye exams are recommended.
- Weight Gain: Expect potential weight gain due to fluid retention and altered metabolism. A balanced diet and exercise are crucial.
Important Note: This information is not exhaustive. Always discuss potential side effects and complications with your doctor before and during treatment. Your healthcare provider can provide personalized advice based on your medical history and the specific treatment plan.
Monitoring and Management of Adverse Reactions
Closely monitor patients receiving Prednisone 1000 mg IV for common adverse effects. Regularly assess vital signs, including blood pressure, heart rate, and respiratory rate. Pay close attention to fluid balance; weigh patients daily.
- Hyperglycemia: Check blood glucose levels frequently, especially in diabetic patients. Adjust insulin or oral hypoglycemics as needed. Consider frequent small meals.
- Hypokalemia: Monitor serum potassium levels. Supplement potassium if needed, following laboratory guidance. Consider dietary adjustments.
- Gastrointestinal distress: Administer medication with food to minimize nausea and vomiting. Antacids or H2 blockers may be helpful. Consider a low-fat, easily digestible diet.
- Fluid retention: Monitor for edema, weight gain, and shortness of breath. Restrict sodium intake and encourage fluid restriction as per medical guidelines.
- Infection: Monitor for signs and symptoms of infection, such as fever, chills, and changes in white blood cell count. Prophylactic antibiotics might be indicated in high-risk patients. Encourage meticulous hand hygiene.
- Mood changes: Assess patients for anxiety, depression, or insomnia. Psychiatric consultation may be necessary. Closely monitor for suicidal ideation.
- Increased risk of bleeding: Monitor for signs of bleeding, including bruising, bleeding gums, and gastrointestinal bleeding. Consider platelet count monitoring. Avoid concomitant use with anticoagulants if possible.
Document all adverse reactions meticulously. Adjust the dosage or discontinue Prednisone based on the severity of adverse reactions and clinical judgment. Promptly address any serious adverse effects. Consult with a specialist as needed. A gradual tapering schedule is generally recommended when discontinuing Prednisone to minimize withdrawal symptoms.
- Regularly assess patient response to treatment. Adjust treatment as clinically indicated.
- Provide thorough patient education regarding potential adverse effects and their management.
- Ensure patient understands the importance of adhering to the prescribed medication regimen and follow-up appointments.
Patient Education and Support
Understand your Prednisone treatment: High-dose intravenous Prednisone (1000mg) is potent. It effectively reduces inflammation but carries potential side effects. Your doctor will explain your specific dosage and duration.
Monitor for side effects: Watch for increased thirst, frequent urination, weight gain, mood changes, and swelling. Report any unusual symptoms immediately to your doctor or nurse. These can be managed with adjustments to your treatment.
Managing Side Effects
Dietary changes can help: Eat a balanced diet low in sodium to manage fluid retention. Consume potassium-rich foods like bananas and spinach to counter potassium loss. Maintain a healthy weight through proper nutrition and exercise.
Lifestyle adjustments are key: Get adequate rest. Avoid strenuous activity, especially during initial treatment. Manage stress through relaxation techniques like deep breathing.
Medication and Follow-up
Take other medications as prescribed: Do not stop any other medications without consulting your doctor. Prednisone can interact with other drugs.
Schedule follow-up appointments: Your doctor will schedule regular checkups to monitor your progress and adjust your treatment as needed. Attendance at these appointments is vital.
| Potential Side Effect | What to Do |
|---|---|
| Increased thirst/urination | Drink plenty of water; notify your doctor |
| Weight gain | Follow a balanced diet; consult a nutritionist |
| Mood changes | Communicate with your doctor or therapist; use stress-reducing techniques. |
| Swelling | Elevate affected limbs; report to your doctor immediately |
Ask questions: Don’t hesitate to ask your healthcare team any questions you have about your treatment. Clarify any concerns you may have about potential side effects or medication management. Your understanding is paramount.
Interactions with Other Medications
Prednisone 1000 mg IV can interact significantly with various medications. Always inform your doctor about all medications you are taking, including over-the-counter drugs, supplements, and herbal remedies. This helps avoid potentially dangerous interactions.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Combining prednisone with NSAIDs, such as ibuprofen or naproxen, increases the risk of stomach ulcers and bleeding. Your doctor might recommend alternative pain relief options.
Blood Thinners
Prednisone can interact with blood thinners like warfarin, increasing bleeding risk. Close monitoring of your blood clotting time is necessary. Dosage adjustments may be required.
Diabetes Medications
Prednisone can elevate blood sugar levels, potentially requiring adjustments to your diabetes medications. Regular blood sugar monitoring is vital.
Potassium-Depleting Diuretics
Concurrent use of prednisone and potassium-depleting diuretics can lead to dangerously low potassium levels (hypokalemia). Your doctor will monitor your potassium levels and may prescribe potassium supplements.
Immunosuppressants
Combining prednisone with other immunosuppressants increases the risk of infections. Your doctor will carefully assess the risks and benefits before combining these medications.
This information is not exhaustive. Consult your doctor or pharmacist for a complete list of potential drug interactions and personalized advice.
Long-Term Implications and Tapering Strategies
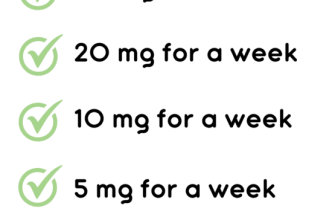
High-dose prednisone (1000 mg IV) carries significant risks with prolonged use. Expect potential side effects like osteoporosis, increased risk of infection, impaired wound healing, and hyperglycemia. Monitoring blood glucose and bone density is crucial.
Tapering is absolutely necessary to minimize these risks. A slow, gradual reduction is key. Avoid abrupt cessation. A common strategy involves reducing the dose by 5-10 mg every few days, adjusting based on patient response and monitoring for withdrawal symptoms like fatigue, muscle weakness, or joint pain.
| Daily Dose (mg) | Reduction Strategy (Example) |
|---|---|
| 1000 | Reduce by 10mg every 3 days |
| 900 | Reduce by 10mg every 3 days |
| 800 | Reduce by 5mg every 3 days |
| 700 | Reduce by 5mg every 3 days |
| … | Continue decreasing dose until complete cessation |
The tapering schedule should be individualized and closely monitored by a physician. Regular blood work, including complete blood count and metabolic panel, helps assess the patient’s response to the medication and guide adjustments in the tapering process. Consider consulting an endocrinologist for ongoing management of potential long-term effects.
Remember, individual responses vary considerably. Close collaboration with the healthcare team ensures a safe and effective tapering process.