Prednisone frequently causes leukocytosis, a rise in white blood cell count. This increase is typically a predictable side effect, often reflecting a steroid-induced increase in neutrophils. Understanding this relationship is crucial for accurate interpretation of blood tests.
Monitor your white blood cell count regularly if you are prescribed prednisone, particularly during the initial phases of treatment and any dose adjustments. Significant elevations warrant discussion with your physician. They will likely assess the clinical picture, considering symptoms and other factors, to differentiate between a benign steroid-induced effect and a potential underlying infection or other complication.
Remember: a simple elevated white blood cell count doesn’t automatically mean there’s a serious problem. However, proactive monitoring and open communication with your healthcare provider are key to managing this medication effectively and ensuring your wellbeing. Your doctor can help determine the significance of any changes in your blood count.
Specific blood work recommendations should come from your physician based on your individual health status and treatment plan. This information aims to increase understanding, not replace professional medical advice.
- Leukocytosis and Prednisone: A Detailed Overview
- Understanding Leukocytosis: Types and Causes
- Causes Beyond Infection
- Identifying the Root Cause
- Prednisone’s Mechanism of Action and Impact on Blood Cells
- Leukocytosis as a Side Effect of Prednisone: Incidence and Severity
- Differentiating Prednisone-Induced Leukocytosis from Other Causes
- Monitoring Leukocyte Counts During Prednisone Treatment
- Managing Prednisone-Induced Leukocytosis: Treatment Strategies
- Investigating the Cause
- Treatment Approaches
- Prednisone Dose Adjustment
- Alternative Medications (If Necessary)
- Monitoring and Follow-up
- Disclaimer:
- Potential Complications of High Leukocyte Counts on Prednisone
- Infection Risk
- Impact on Prednisone Efficacy
- Other Potential Complications
- Treatment Adjustments
- Regular Monitoring
- When to Seek Medical Attention Regarding Leukocytosis and Prednisone
Leukocytosis and Prednisone: A Detailed Overview
Prednisone, a corticosteroid, frequently causes leukocytosis, an elevation in white blood cell count. This increase primarily affects neutrophils, a type of white blood cell crucial for fighting infection. The mechanism involves stimulating the bone marrow to release more neutrophils into circulation. This effect is usually dose-dependent, meaning higher prednisone doses tend to lead to more pronounced leukocytosis.
Clinicians monitor complete blood counts (CBCs) to track this effect. A significant rise in white blood cells warrants careful evaluation. While often benign, it can mask an underlying infection, making diagnosis more challenging. Therefore, if a patient on prednisone develops symptoms of infection (fever, cough, etc.), a thorough investigation is crucial, even with elevated white blood cell counts.
Differentiation is key. Leukocytosis due to prednisone typically shows a predominance of neutrophils. Other causes of leukocytosis, like infections or leukemia, may present different white blood cell profiles. A detailed blood analysis, including differential counts, helps distinguish between prednisone-induced leukocytosis and other conditions.
Managing this side effect involves careful monitoring and dose adjustment of prednisone when possible. The physician should weigh the benefits of prednisone against the potential risks. In some instances, alternative medications may be considered. Always consult a healthcare professional to manage prednisone-induced leukocytosis.
Remember, self-treating is never advised. A healthcare provider can accurately interpret blood test results, assess the patient’s overall health, and determine the best course of action, whether it’s monitoring the leukocytosis, adjusting the prednisone dose, or exploring alternative therapies.
Understanding Leukocytosis: Types and Causes
Leukocytosis signifies a high white blood cell count. Several types exist, each reflecting a different underlying cause. Neutrophilia, the most common, involves increased neutrophils, often indicating bacterial infection, inflammation, or stress. Lymphocytosis, elevated lymphocytes, frequently signals viral infections or certain cancers. Monocytosis highlights increased monocytes, possibly suggesting chronic inflammation or certain infections. Eosinophilia, characterized by elevated eosinophils, often points to allergic reactions, parasitic infections, or certain cancers. Basophilia, an increase in basophils, can be associated with allergic reactions, autoimmune diseases, and certain blood cancers.
Causes Beyond Infection
Many factors besides infection trigger leukocytosis. Medications like prednisone, commonly used to suppress the immune system, can elevate white blood cell counts. Autoimmune diseases, such as rheumatoid arthritis and lupus, often lead to leukocytosis due to ongoing inflammation. Stress and certain cancers can also increase white blood cell production. Finally, some blood disorders directly impact white blood cell formation, leading to elevated counts. Accurate diagnosis requires considering all possible contributors and further investigation.
Identifying the Root Cause
Determining the cause of leukocytosis is crucial for appropriate treatment. A complete blood count (CBC) with differential provides essential information, identifying the specific type of elevated white blood cells. Further tests, including imaging studies, blood cultures, and other specialized assessments, may help pinpoint the underlying cause. Your doctor will guide you through the necessary steps.
Prednisone’s Mechanism of Action and Impact on Blood Cells
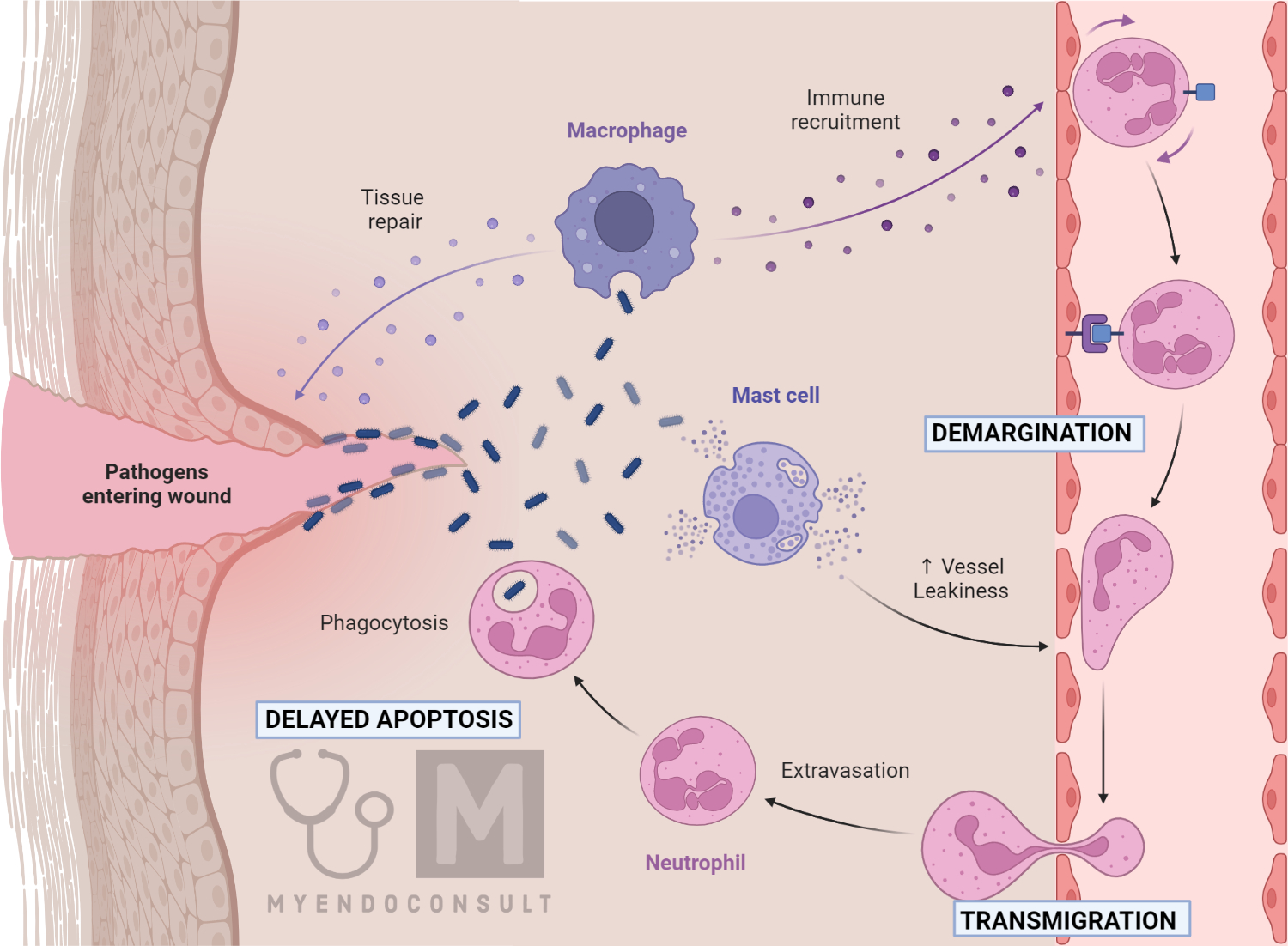
Prednisone, a glucocorticoid, exerts its effects by binding to intracellular glucocorticoid receptors. This complex then translocates to the nucleus, modulating gene transcription. Specifically, it influences the production and function of various immune cells.
Regarding leukocytosis, prednisone initially can cause a transient increase in white blood cell count, particularly neutrophils. This happens because prednisone reduces inflammation and redistributes neutrophils from the marginal pools in the blood vessels to the circulating blood. However, long-term prednisone use frequently leads to immunosuppression. This results in a decrease in circulating lymphocytes, monocytes, eosinophils, and basophils.
The impact on individual blood cell lineages varies. For instance, while prednisone increases the number of circulating neutrophils temporarily, it can also decrease their lifespan and function in the long run. Conversely, prolonged prednisone therapy significantly suppresses lymphocytes, potentially increasing susceptibility to infections. Therefore, monitoring blood cell counts is crucial during prednisone therapy.
Remember that the effects of prednisone on blood cells depend on factors like dosage, duration of treatment, and the patient’s individual response. A healthcare professional should carefully monitor blood counts and adjust treatment accordingly. Unexpected changes require prompt medical attention.
Leukocytosis as a Side Effect of Prednisone: Incidence and Severity
Prednisone, a commonly used corticosteroid, frequently causes leukocytosis, an increase in white blood cell count. Studies show the incidence varies greatly depending on the dose and duration of prednisone treatment, as well as the patient’s underlying health conditions. For example, one study reported leukocytosis in up to 80% of patients receiving high-dose prednisone therapy. However, milder doses often yield a much lower incidence.
The severity of prednisone-induced leukocytosis also varies considerably. While often mild and asymptomatic, it can sometimes lead to significant elevations in white blood cell counts. This is particularly true with prolonged high-dose use. Such significant increases warrant close monitoring, especially in patients with a history of hematological disorders. Regular complete blood counts (CBCs) are recommended to track white blood cell levels during prednisone treatment.
Neutrophilia, an increase in neutrophils (a type of white blood cell), is the most common type of leukocytosis observed with prednisone. Lymphopenia (a decrease in lymphocytes) may also occur, although less frequently than neutrophilia. Clinicians should assess both neutrophil and lymphocyte counts, considering the potential for immunosuppression with high-dose prednisone.
Management strategies typically focus on careful monitoring of blood counts and adjusting prednisone dosage if necessary. In cases of severe leukocytosis, the physician might reduce the prednisone dose or consider alternative treatment options. Always consult your doctor for concerns related to changes in your blood work during prednisone treatment. They can provide personalized recommendations based on your specific health needs.
Differentiating Prednisone-Induced Leukocytosis from Other Causes
First, carefully review the patient’s medication history. Prednisone, a glucocorticoid, characteristically causes a neutrophilic leukocytosis, often with a left shift (increased immature neutrophils). This typically presents as a mild to moderate increase in the total white blood cell count, primarily driven by neutrophils.
Contrast this with other causes: Infections frequently lead to leukocytosis with a higher proportion of lymphocytes or bands, depending on the type of infection. Similarly, inflammatory conditions like rheumatoid arthritis may present with leukocytosis, but often accompanied by other inflammatory markers like elevated ESR or CRP. Malignancies usually result in more significant and variable leukocytosis, potentially involving abnormal cell types. Consider a complete blood count (CBC) with differential to assess the specific cell populations involved.
Specific findings to distinguish prednisone-induced leukocytosis: A predominantly neutrophilic leukocytosis with a left shift in the absence of infection or inflammatory symptoms strongly suggests prednisone as the culprit. Moreover, the temporal relationship is critical; leukocytosis usually appears within days to weeks of starting prednisone and resolves after discontinuation.
Further investigation: If the leukocytosis is severe, unexplained, or persistent despite prednisone cessation, further evaluation is warranted to rule out other causes. This might involve examining peripheral blood smears, assessing other inflammatory markers, and conducting imaging studies depending on clinical suspicion. For instance, consider a bone marrow biopsy if malignancy is suspected.
In summary: A thorough medication review, CBC with differential, and careful assessment of the clinical context are necessary to differentiate prednisone-induced leukocytosis from other causes. Always consider the temporal relationship between medication use and the onset of leukocytosis. If uncertainty remains, additional diagnostic tests can provide further clarity.
Monitoring Leukocyte Counts During Prednisone Treatment
Regularly schedule blood tests to track your leukocyte count. Frequency depends on your individual health and prednisone dosage; discuss this with your doctor. Baseline counts are crucial before starting prednisone.
Expect some increase in leukocytes, especially neutrophils, initially. This is a common effect of prednisone. However, significant or sustained increases warrant immediate medical attention.
Monitor for signs of infection alongside leukocyte monitoring. Fever, chills, or localized inflammation should prompt immediate testing. These symptoms can be masked by prednisone’s anti-inflammatory effects.
Closely follow your doctor’s instructions regarding dosage and duration of prednisone. Adjustments to the dosage may be necessary based on your leukocyte response and overall health.
Maintain open communication with your healthcare provider. Report any unusual symptoms or concerns promptly. This collaborative approach ensures safe and effective management of your treatment.
Document all blood test results and share them with your physician. This helps in tracking changes and making informed decisions about your treatment plan. Keeping records aids in detecting potential issues early.
Managing Prednisone-Induced Leukocytosis: Treatment Strategies
First, carefully assess the severity of leukocytosis. Mild elevations often require no specific treatment beyond monitoring, especially if other symptoms are absent. However, significant increases warrant further investigation.
Investigating the Cause
Before initiating treatment, pinpoint the underlying cause. Is the leukocytosis solely due to prednisone, or are there other contributing factors, such as infection or another underlying condition?
- Complete blood count (CBC) with differential: This helps identify the specific type of white blood cells elevated.
- Inflammatory markers (CRP, ESR): Useful for detecting infection or inflammation.
- Other relevant tests: Depending on clinical presentation, consider further investigations, such as blood cultures or imaging studies.
Treatment Approaches
Treatment focuses on addressing the underlying cause. If infection is present, appropriate antibiotics or antivirals are crucial. If another medical condition contributes, treating that condition is paramount.
Prednisone Dose Adjustment
In cases where prednisone is the primary driver, consider cautiously reducing the dosage. This must be done gradually under close medical supervision to avoid adrenal insufficiency. Never abruptly discontinue prednisone.
Alternative Medications (If Necessary)
- In rare situations with severe, intractable leukocytosis despite prednisone dose reduction, your doctor might consider alternative immunosuppressants. This decision should be made on a case-by-case basis given potential side effects.
- Consult a hematologist or oncologist for specialized management of severe or complicated cases.
Monitoring and Follow-up
- Regular blood tests are essential to monitor leukocyte counts and overall blood cell parameters.
- Closely monitor the patient for symptoms of infection or other complications. Report any changes immediately.
- Continue regular follow-up appointments to assess the effectiveness of the chosen treatment approach and adjust as needed.
Disclaimer:
This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for diagnosis and treatment of any medical condition.
Potential Complications of High Leukocyte Counts on Prednisone
Monitoring leukocyte counts during prednisone treatment is vital. High leukocyte counts, even with prednisone, can signal underlying infections or other serious conditions. Prompt identification and management are crucial.
Infection Risk
Elevated white blood cell counts might indicate an active infection. Prednisone suppresses the immune system, potentially masking infection symptoms. This combination increases the risk of severe infections if left untreated. Regular blood tests and careful monitoring for symptoms such as fever, chills, or localized inflammation are necessary.
Impact on Prednisone Efficacy
High leukocyte counts don’t always directly impact prednisone’s effectiveness in treating the primary condition. However, the underlying cause of elevated leukocytes needs addressing. An untreated infection, for instance, could compromise treatment success. The physician must determine the cause of the high leukocyte count to optimize treatment.
Other Potential Complications
While less common, persistently high leukocyte counts during prednisone treatment could point towards conditions like leukemia or other hematological disorders. Therefore, a thorough evaluation, potentially including a bone marrow biopsy, may be needed depending on the patient’s medical history and other symptoms.
Treatment Adjustments
Managing high leukocyte counts often involves addressing the underlying cause. This may necessitate antibiotics for infections, adjustments to the prednisone dosage (under strict medical supervision), or treatment for specific hematological disorders. Never alter your medication without consulting your physician.
| Possible Cause | Associated Symptoms | Treatment Considerations |
|---|---|---|
| Bacterial Infection | Fever, chills, localized pain | Antibiotics, supportive care |
| Viral Infection | Fever, fatigue, cough, body aches | Supportive care, antiviral medication (if applicable) |
| Leukemia/Lymphoma | Fatigue, weight loss, swollen lymph nodes | Oncology consultation, chemotherapy, targeted therapy |
Regular Monitoring
Regular blood tests are crucial to monitor leukocyte counts and overall health during prednisone treatment. Prompt reporting of any new or worsening symptoms to your physician is vital for timely intervention.
When to Seek Medical Attention Regarding Leukocytosis and Prednisone
Contact your doctor immediately if you experience any of the following symptoms alongside leukocytosis while taking prednisone:
- Fever of 100.4°F (38°C) or higher
- Severe fatigue or weakness
- Unexplained weight loss
- Night sweats
- Swollen lymph nodes
- Easy bruising or bleeding
- Recurring infections
- Shortness of breath
- Chest pain
- Persistent cough
Seek immediate medical attention if your leukocyte count significantly increases after starting prednisone, or if it remains high despite adjustments in your medication.
Regular blood tests are critical to monitor your leukocyte count while on prednisone. Report any abnormal results to your healthcare provider without delay. Prompt action can prevent serious complications.
- Schedule a follow-up appointment as directed by your doctor to discuss your blood test results and adjust your treatment plan as needed.
- Maintain open communication with your healthcare team about any concerns or changes in your health status.
- Always follow your doctor’s instructions regarding medication dosage and schedule.
Remember, early intervention is key in managing potential complications associated with leukocytosis and prednisone.