Prednisone usually helps control hives, but sometimes it doesn’t. If your hives persist despite prednisone treatment, consider alternative approaches. A detailed allergy test can pinpoint specific triggers, guiding more effective avoidance strategies. This can significantly reduce the frequency and severity of future outbreaks.
Beyond allergy testing, your doctor might suggest other medications. Second-generation antihistamines, like cetirizine or fexofenadine, often prove beneficial when used alongside or instead of prednisone. In more severe cases, stronger medications such as omalizumab or dupilumab might be necessary. Discuss these options with your physician to determine the best course of action for your specific situation.
Managing your environment is equally crucial. Identifying and eliminating potential irritants within your home is key. Common culprits include dust mites, pet dander, and certain cleaning products. Simple lifestyle changes, like regular washing of bedding and clothes and switching to hypoallergenic cleaning products, can dramatically decrease hive occurrences. Remember to meticulously document potential triggers and their impact to help your doctor tailor a treatment plan.
Regular communication with your doctor is paramount. Describe your symptoms in detail, including their severity, duration, and any associated factors. Providing this information enables your doctor to make informed decisions and adjust your treatment as needed. Don’t hesitate to contact your healthcare provider if your condition worsens or doesn’t improve.
- Hives Not Responding to Prednisone: Understanding and Addressing Treatment Failure
- Identifying Potential Underlying Causes of Prednisone Ineffectiveness
- Alternative Treatment Options for Chronic Urticaria
- Investigating Other Allergens and Triggers Beyond Initial Diagnosis
- Environmental Factors
- Medical Conditions
- The Role of Diagnostic Testing in Refining Treatment Strategies
- When to Seek Specialized Care for Refractory Hives
Hives Not Responding to Prednisone: Understanding and Addressing Treatment Failure
If your hives aren’t improving with prednisone, seek immediate medical attention. This isn’t uncommon, and several factors could be at play.
First, ensure the diagnosis is accurate. Urticaria mimics other conditions. A dermatologist or allergist might order additional tests, like blood work to check for autoimmune disorders or infections. This might include checking for thyroid issues or other underlying health problems.
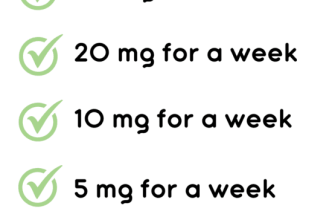
Second, consider the dosage and duration of your prednisone treatment. Insufficient prednisone may fail to control the hives. Your doctor might adjust your dosage or extend the treatment period. They may prescribe alternative medications such as antihistamines. Your doctor may prescribe a higher dose for a short period then slowly taper off the prednisone.
Third, identify potential triggers. Common culprits include food allergies, medications, insect bites, stress, and infections. Keeping a detailed diary of your symptoms and activities can help pinpoint these triggers, enabling proactive avoidance. This detailed tracking, combined with doctor’s input, is crucial for management.
Fourth, consider alternative or additional medications. Antihistamines, such as cetirizine or fexofenadine, often work alongside prednisone. In severe cases, other treatments, like omalizumab or dupilumab, may be necessary. Discuss these options with your doctor to find the best approach.
Fifth, explore underlying medical conditions. Sometimes, hives signal a more significant problem. Conditions such as lupus, thyroid disease, or lymphoma might manifest as hives. Testing can identify and address these underlying issues, improving the hives.
Finally, consistent communication with your healthcare provider is vital. Regular check-ups allow for prompt adjustments to your treatment plan, ensuring you receive the best possible care and improve your quality of life.
Identifying Potential Underlying Causes of Prednisone Ineffectiveness
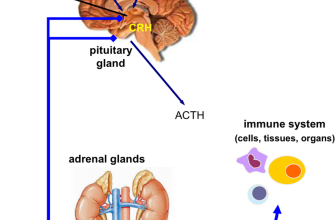
First, consider alternative diagnoses. Urticaria, often treated with prednisone, might actually stem from underlying conditions like autoimmune diseases (e.g., lupus, rheumatoid arthritis), infections (e.g., viral hepatitis, mononucleosis), or even certain cancers. Detailed blood tests and imaging studies can clarify this.
Second, assess medication interactions. Some drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, can interfere with prednisone’s efficacy. A thorough medication review is vital.
Third, examine your prednisone regimen. Insufficient dosage or improper administration can hinder results. Consult your doctor to ensure the correct dose and frequency are being used.
Fourth, explore other potential triggers. Contact dermatitis from specific substances, food allergies (e.g., peanuts, shellfish), or insect bites might be responsible. Detailed allergy testing can pinpoint the cause.
Finally, investigate the possibility of prednisone resistance. While rare, some individuals exhibit reduced responsiveness to the medication. Your doctor might explore alternative treatment options, like second-line antihistamines (e.g., omalizumab), immunomodulators, or biologics, in such cases.
| Possible Cause | Investigative Steps |
|---|---|
| Underlying Autoimmune Disease | Blood tests (ANA, anti-dsDNA, rheumatoid factor) |
| Infection | Complete blood count (CBC), liver function tests, specific infection tests |
| Medication Interaction | Detailed medication review |
| Allergic Reaction | Allergy testing (skin prick, blood tests) |
| Prednisone Resistance | Discussion with your doctor regarding alternative treatments |
Alternative Treatment Options for Chronic Urticaria
If prednisone isn’t providing sufficient relief, explore these options:
- Second-generation H1 antihistamines: Consider increasing the dosage of your current H1 antihistamine or switching to a second-generation option like fexofenadine, cetirizine, or levocetirizine. Doctors often prescribe higher-than-usual doses for chronic urticaria.
- H2 antihistamines: Combining an H1 antihistamine with an H2 antihistamine, such as ranitidine or famotidine, can significantly improve symptom control in some individuals.
- Omalizumab: This monoclonal antibody targets immunoglobulin E (IgE), a key player in allergic reactions. It’s a highly effective treatment for severe, chronic urticaria that doesn’t respond to other therapies. Discuss this option with your allergist or dermatologist.
- Leukotriene inhibitors: Medications like montelukast or zafirlukast can help reduce inflammation and may provide additional benefits when used alongside antihistamines.
- Cyclosporine: This immunosuppressant is reserved for severe cases unresponsive to other treatments. It carries potential side effects, necessitating careful monitoring by a physician.
Beyond medication, lifestyle adjustments can help manage symptoms:
- Identify and avoid triggers: Keep a detailed diary noting food, environmental factors, or stressors that correlate with flare-ups. This allows for targeted avoidance.
- Stress management: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises. Stress frequently exacerbates hives.
- Regular exercise and a healthy diet: Maintaining a healthy lifestyle contributes to overall well-being and may indirectly improve symptom control.
Remember, finding the right treatment often involves a process of trial and error. Close collaboration with your doctor is crucial to managing your chronic urticaria effectively.
Investigating Other Allergens and Triggers Beyond Initial Diagnosis
If your hives aren’t responding to prednisone, expand your allergen investigation. Consider food sensitivities beyond common culprits. Keep a detailed food diary, noting reactions. Skin prick tests offer a quick assessment for common inhalant allergens like pollen, pet dander, and dust mites. Consider a comprehensive panel for less common allergens.
Environmental Factors
Examine your environment. New cleaning products, cosmetics, or fabrics can trigger hives. Assess exposure to potential irritants at work or home. Monitor weather changes; some individuals experience hive flares with temperature or humidity fluctuations. Regularly wash bedding in hot water to reduce dust mite exposure. Analyze your water source for unusual contaminants. If you suspect a work-related trigger, consult your occupational health professional.
Medical Conditions
Certain medical conditions, such as autoimmune diseases or thyroid issues, can manifest as chronic hives. Discuss other symptoms with your doctor to explore underlying medical factors. Your doctor might order blood tests to check for these conditions. A thorough review of your medications is also necessary, as some drugs can induce hives as a side effect.
The Role of Diagnostic Testing in Refining Treatment Strategies
If prednisone isn’t controlling your hives, further investigation is necessary. A detailed allergy assessment, including skin prick testing and specific IgE blood tests, identifies potential triggers like pollen, pet dander, or foods. This pinpoints avoidance strategies and potential immunotherapy.
Consider blood tests for autoimmune disorders like lupus or thyroid disease, which can cause hives. Autoimmune markers, such as antinuclear antibodies (ANA) and antithyroid antibodies, help guide treatment.
A complete blood count (CBC) can reveal infections or other underlying conditions contributing to the hives. Elevated white blood cell counts might indicate infection requiring targeted treatment.
If your doctor suspects a hereditary condition or a rare cause, genetic testing or specialized investigations might be recommended. This helps tailor management to the specific genetic factors involved.
Biopsy of a hive lesion can sometimes provide diagnostic clues. Histopathology can differentiate between urticaria and other skin conditions, improving treatment accuracy.
Regular follow-up appointments allow monitoring of treatment response and adjustments based on test results. This ensures you receive the most appropriate and personalized care.
When to Seek Specialized Care for Refractory Hives
Contact an allergist or dermatologist if your hives persist despite prednisone treatment for longer than two weeks. This timeline provides a practical guideline; individual situations may vary.
Consider specialized care if: your hives are severe, causing significant distress or impacting your daily life. This includes difficulty breathing, swelling of the face or throat (angioedema), or widespread skin involvement.
Seek immediate medical attention if you experience these symptoms.
If your hives are unresponsive to several different treatments, including antihistamines and prednisone, a specialist can help identify underlying causes and explore alternative therapies. This may include investigating autoimmune conditions, infections, or other less common triggers.
A specialist can perform thorough allergy testing, potentially revealing specific allergens responsible for your hives. They can also adjust medication regimens and offer other management strategies, such as biologics or omalizumab, depending on your individual needs.
Don’t hesitate to seek a second opinion if you’re unsatisfied with your current treatment. A fresh perspective can often lead to a more successful outcome.