Regularly monitor your kidney function if you’re prescribed prednisone, especially if you have pre-existing conditions. Prednisone, a potent corticosteroid, can negatively impact kidney health, potentially accelerating the progression of chronic kidney disease (CKD). This isn’t always the case, but proactive monitoring is key.
Schedule regular blood tests to measure your glomerular filtration rate (GFR) and creatinine levels. These tests provide crucial insights into your kidney’s filtering capacity. Aim for at least yearly check-ups, or more frequently as your doctor advises, based on your individual risk profile and response to treatment. Early detection of kidney problems allows for timely interventions.
Open communication with your physician is paramount. Discuss your complete medical history, including any family history of kidney disease, before starting prednisone treatment. Report any new or worsening symptoms, such as swelling, fatigue, or changes in urination patterns, immediately. Your doctor can adjust your medication or suggest supportive therapies based on your specific needs.
Consider lifestyle modifications to support kidney health. Maintaining a healthy weight, following a balanced diet low in sodium and protein (as recommended by your doctor), and staying well-hydrated can help minimize the strain on your kidneys. Regular exercise, as tolerated, further promotes overall well-being and can help manage conditions linked to CKD. Remember, these measures are complementary to medical care, not replacements.
- Chronic Kidney Disease and Prednisone: A Detailed Look
- Monitoring Kidney Function
- Dosage and Administration
- Potential Side Effects
- Alternative Treatments
- Comparison of Prednisone and Alternative Treatments in CKD
- Prednisone’s Impact on Kidney Function
- CKD Stages and Prednisone Use: Risk Assessment
- Monitoring Kidney Health During Prednisone Treatment
- Understanding Your Test Results
- Beyond Blood and Urine: Staying Hydrated
- Lifestyle Modifications
- Alternative Medications to Prednisone for CKD Patients
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Biologics and Targeted Therapies
- Monitoring Renal Function
- Individualized Treatment Plans
- Lifestyle Modifications to Mitigate Prednisone’s Renal Effects
- Long-Term Outlook: Managing CKD and Prednisone
- Dietary Adjustments
- Lifestyle Modifications
- Medication Management
- Long-Term Goals
Chronic Kidney Disease and Prednisone: A Detailed Look
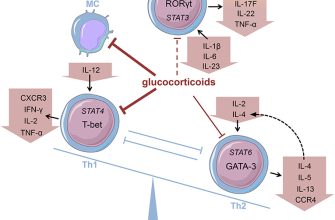
Prednisone, a corticosteroid, can worsen kidney function in individuals with chronic kidney disease (CKD). This is because prednisone affects electrolyte balance, potentially increasing blood pressure and damaging kidney structures. Doctors carefully weigh the benefits of prednisone against these risks before prescribing it for patients with CKD.
Monitoring Kidney Function
Regular monitoring of kidney function is vital when a patient with CKD is prescribed prednisone. Blood tests (creatinine and eGFR) and urine tests are frequently used to assess kidney health. These tests help determine the prednisone dosage and identify potential complications early.
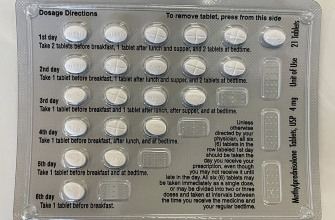
Dosage and Administration
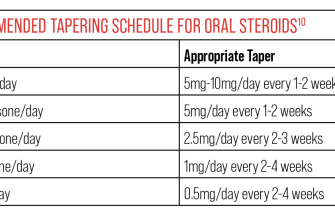
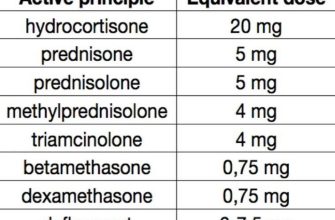
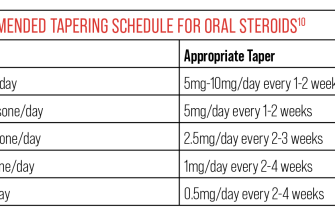
Prednisone dosage for CKD patients is significantly lower than for patients without kidney problems. The lowest effective dose is crucial to minimize potential kidney damage. Doctors tailor the dosage and duration based on the individual’s specific condition and kidney function. The route of administration (oral or intravenous) depends on the patient’s needs and the severity of their condition.
Potential Side Effects
Patients should be aware of potential side effects, which include increased blood pressure, fluid retention, and increased blood sugar. Regular monitoring of these parameters is needed. Immediate medical attention is required if you experience severe side effects. These side effects could be particularly dangerous for people with advanced CKD.
Alternative Treatments
In cases where the benefits of prednisone don’t outweigh the risks for a CKD patient, alternative treatments will be explored. These alternatives depend entirely on the underlying condition requiring prednisone. Your doctor will work with you to find the safest and most effective treatment plan.
Comparison of Prednisone and Alternative Treatments in CKD
| Treatment | Kidney Impact | Other Side Effects | Suitable for CKD? |
|---|---|---|---|
| Prednisone (low dose) | Potential for worsening of function | Increased blood pressure, fluid retention, hyperglycemia | Sometimes, with close monitoring |
| Other immunosuppressants (e.g., mycophenolate mofetil) | Variable, less likely to worsen function than prednisone | Gastrointestinal upset, bone marrow suppression | Often preferred over prednisone |
| Non-pharmacological treatments | Often beneficial for overall kidney health | Variable, depending on the treatment | Always recommended in addition to medication |
Remember, this information is for general knowledge and does not constitute medical advice. Always consult your physician regarding treatment options for your specific situation.
Prednisone’s Impact on Kidney Function
Prednisone, a common corticosteroid, can affect kidney function in several ways. High doses or prolonged use increase the risk of fluid retention, leading to high blood pressure and swelling. This fluid overload strains the kidneys.
Prednisone also raises blood sugar levels. Sustained hyperglycemia damages blood vessels, including those in the kidneys, potentially accelerating kidney disease progression. Careful monitoring of blood glucose is crucial.
Furthermore, prednisone can increase the excretion of calcium, potentially leading to decreased bone density and increasing the risk of kidney stones. Adequate calcium intake, monitored by a physician, is recommended.
The drug may also interact with certain medications used to treat kidney disease. This necessitates close communication with your doctor regarding all medications.
Patients with pre-existing kidney disease should discuss prednisone use with their nephrologist before starting the medication. Regular monitoring of kidney function, including blood tests and urine analysis, is necessary throughout the course of prednisone treatment to detect and manage potential side effects.
Always inform your healthcare provider about your kidney health status and any concerns.
CKD Stages and Prednisone Use: Risk Assessment
Prednisone, a corticosteroid, carries significant risks when used with chronic kidney disease (CKD). The severity of these risks directly correlates with the stage of CKD.
Stage 1-2 CKD: While prednisone use is generally avoided if possible, in these early stages, the risks may be manageable with close monitoring of kidney function (glomerular filtration rate or GFR) and blood pressure. Regular blood tests are crucial to detect any adverse changes. Consider alternative treatments if feasible.
- Monitor GFR at least monthly.
- Closely manage blood pressure.
- Regularly assess for fluid retention and electrolyte imbalances.
Stage 3-4 CKD: Prednisone use presents increased risk here. The potential for worsening kidney function is considerably higher. Weigh the benefits of prednisone against these elevated risks. A nephrologist’s guidance is absolutely necessary before initiating prednisone therapy.
- Expect more frequent GFR and electrolyte monitoring.
- Careful fluid management is critical.
- Closely watch for signs of infection, as prednisone suppresses immunity.
Stage 5 CKD (End-Stage Renal Disease): Prednisone use in this stage is generally contraindicated due to the severe impairment of kidney function. The likelihood of significant complications is very high. Alternative therapies should be strongly considered.
General Recommendations for all CKD stages: Hydration is paramount. Consume a potassium-restricted diet to manage hyperkalemia risk. Always inform your doctor about all medications, including over-the-counter drugs and herbal supplements, to avoid dangerous interactions.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult with a nephrologist or other qualified healthcare professional for personalized guidance regarding prednisone use and CKD management.
Monitoring Kidney Health During Prednisone Treatment
Regular blood and urine tests are key. Your doctor will schedule these to track creatinine and glomerular filtration rate (GFR), crucial indicators of kidney function. Expect these tests at least every few months, potentially more frequently depending on your individual risk factors and response to prednisone. Elevated creatinine or a declining GFR signal potential kidney damage requiring adjustments to your treatment plan.
Understanding Your Test Results
Don’t hesitate to ask your doctor to explain your results clearly. A simple explanation can ease concerns and ensure you understand the implications for your kidney health. These tests provide a quantitative measure of how well your kidneys are functioning. Changes in these values help monitor the drug’s impact and prompt necessary interventions.
Beyond Blood and Urine: Staying Hydrated
Maintaining adequate hydration is vital. Prednisone can increase your risk of dehydration, which further stresses your kidneys. Aim for at least eight glasses of water daily, adjusting this amount based on your activity level and climate. Listen to your body – thirst is a clear signal to drink more.
Lifestyle Modifications
A balanced diet low in sodium and protein can ease the burden on your kidneys. Your physician or a registered dietitian can guide you on creating a personalized diet plan. Regular exercise, within your capabilities, also contributes to overall health and can indirectly support kidney function.
Alternative Medications to Prednisone for CKD Patients
Prednisone’s impact on kidney function necessitates careful consideration in Chronic Kidney Disease (CKD). Fortunately, alternatives exist, depending on the underlying condition requiring steroid treatment. For example, if treating an autoimmune disease, immunosuppressants like mycophenolate mofetil or azathioprine may offer comparable benefits with less nephrotoxicity. These drugs suppress the immune system, thereby reducing inflammation and disease activity.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
For pain or inflammation management, consider NSAID alternatives. Celecoxib, a COX-2 inhibitor, generally poses less risk to kidney function than older NSAIDs like ibuprofen or naproxen. However, always discuss NSAID use with a nephrologist due to potential risks for those with CKD.
Biologics and Targeted Therapies
In certain autoimmune diseases, biologics offer precise targeting of inflammatory pathways, minimizing systemic immunosuppression needed with prednisone. Examples include medications like rituximab or tocilizumab, each having specific applications and potential side effects requiring careful monitoring by a specialist. Always consult with your physician regarding their suitability and potential interactions with existing medications.
Monitoring Renal Function
Regular monitoring of kidney function is vital when considering any medication, particularly alternatives to prednisone. Blood tests, including creatinine and eGFR levels, along with urine analysis, allow for adjustments in medication dosage to maintain renal health. Open communication with your nephrologist is paramount for safe and effective management.
Individualized Treatment Plans
The best alternative to prednisone for a CKD patient depends entirely on the specific clinical scenario. Factors such as the severity of CKD, the underlying condition, and the patient’s overall health significantly influence treatment choices. A collaborative approach involving the patient, nephrologist, and other specialists is critical in tailoring a safe and effective treatment plan.
Lifestyle Modifications to Mitigate Prednisone’s Renal Effects
Managing your diet is key. Reduce sodium intake significantly; aim for less than 2,000 milligrams daily. This helps control blood pressure, a major concern with prednisone and kidney disease.
Increase your potassium intake through fruits and vegetables, but monitor levels with your doctor. Potassium supplements may be necessary depending on your kidney function.
- Prioritize low-sodium, potassium-rich foods like bananas, sweet potatoes, and spinach.
- Limit processed foods, fast food, and restaurant meals, which are often high in sodium.
Staying hydrated is crucial. Drink plenty of water throughout the day to support kidney function. Your doctor can advise on the appropriate amount for your individual needs.
Regular exercise plays a vital role. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This aids in blood pressure control and overall health.
- Choose activities you enjoy to maintain consistency.
- Consult your doctor before starting any new exercise program.
Maintain a healthy weight. Obesity increases the burden on your kidneys. A balanced diet and regular exercise contribute to weight management. Discuss weight loss strategies with your physician.
Manage your blood sugar levels meticulously. Prednisone can affect blood sugar, placing extra strain on your kidneys. Closely monitor your blood glucose and follow your doctor’s guidance on diabetes management.
Quit smoking. Smoking damages blood vessels, further compromising kidney health. Seek support to quit if you need it.
Prioritize adequate sleep. Aim for 7-8 hours of quality sleep each night. Sleep deprivation negatively impacts overall health, including kidney function.
Regularly monitor your blood pressure and kidney function. Follow up with your doctor for scheduled check-ups and blood tests as recommended.
Long-Term Outlook: Managing CKD and Prednisone
Regular monitoring of kidney function is paramount. Schedule frequent blood tests and urine analyses to track creatinine levels, glomerular filtration rate (GFR), and electrolyte balance. Adjust prednisone dosage according to your kidney health and overall response to treatment, always under the close supervision of your nephrologist and rheumatologist.
Dietary Adjustments
A kidney-friendly diet is critical. Reduce protein intake to minimize the strain on your kidneys. Limit potassium, phosphorus, and sodium, consulting a registered dietitian for personalized guidance. Increase your consumption of fruits and vegetables low in potassium, such as apples, cranberries and green beans. Hydration is key; aim for adequate fluid intake while considering restrictions based on your kidney function.
Lifestyle Modifications
Managing blood pressure is extremely important. Follow your doctor’s advice concerning medication and lifestyle changes. Regular exercise, such as brisk walking or swimming, helps maintain cardiovascular health. Smoking cessation is highly recommended as it significantly impacts kidney function. Your doctor can provide guidance on smoking cessation programs.
Medication Management
Closely follow your prescribed medication regimen. Report any side effects to your healthcare team immediately. Consider exploring alternative medications if your doctor deems it necessary, particularly if your kidney function declines. Open communication with your healthcare team is vital. They can provide detailed information on managing potential drug interactions.
Long-Term Goals
The goal is to minimize the negative impact of both CKD and prednisone on your overall health. Active participation in your care, adhering to medical advice, and establishing a strong relationship with your healthcare team can significantly improve your long-term outlook. Regular check-ups and open communication with your doctors will help you achieve the best possible outcomes.