No, prednisone itself doesn’t directly cause osteoarthritis. However, long-term use of this powerful steroid medication can significantly increase your risk of developing or worsening existing osteoarthritis. This is because prednisone impacts bone density and metabolism, creating conditions favorable for joint degradation.
Studies show a correlation between prolonged prednisone treatment and increased incidence of avascular necrosis (bone death), a condition often leading to osteoarthritis. This risk rises with higher doses and longer treatment durations. Factors such as age, pre-existing conditions, and genetics influence the severity of this side effect.
Therefore, it’s critical to discuss the potential risks with your physician before starting or continuing prednisone treatment, especially if you have a family history of osteoarthritis or other bone conditions. Regular monitoring of bone health through bone density scans can be beneficial for those on long-term prednisone therapy. Your doctor might recommend lifestyle modifications, such as weight management and exercise, to mitigate the risk.
Remember, open communication with your healthcare provider is key. They can assess your individual risk factors and help you develop a management plan that balances the benefits of prednisone with potential risks to your bone health. Always prioritize informed decision-making regarding your health.
- Can Prednisone Cause Osteoarthritis?
- Prednisone’s Impact on Bone Health
- Risk Factors and Mitigation
- Alternatives and Management
- Conclusion
- Prednisone’s Effects on Bone Health: A Closer Look
- Decreased Bone Formation
- Increased Bone Resorption
- Practical Implications & Recommendations
- Monitoring for Osteoporosis
- Prednisone and the Risk of Osteoporosis: Understanding the Connection
- How Prednisone Affects Bone Health
- Protecting Your Bones While on Prednisone
- Can Prednisone Exacerbate Existing Osteoarthritis?
- Increased Bone Loss
- Muscle Weakness
- Impact on Cartilage
- Managing the Risks
- Consult Your Doctor
- Studies Linking Long-Term Prednisone Use and Joint Problems
- Avascular Necrosis and Prednisone
- Osteoporosis and Prednisone-Induced Joint Pain
- Other Joint Issues
- Protecting Your Joints While on Prednisone: Lifestyle and Dietary Recommendations
- Nutrition for Joint Health
- Additional Tips
Can Prednisone Cause Osteoarthritis?
Prednisone, while effective for reducing inflammation, doesn’t directly cause osteoarthritis. However, long-term prednisone use increases your risk of developing or worsening existing osteoarthritis. This is because prednisone affects bone health in several ways.
Prednisone’s Impact on Bone Health
High doses of prednisone for extended periods can weaken bones, making them more prone to fractures. This effect, known as steroid-induced osteonecrosis (bone death), can damage joints and accelerate osteoarthritis progression. Reduced bone density also increases the likelihood of joint injury which can trigger or worsen osteoarthritis.
Risk Factors and Mitigation
The risk of developing bone problems from prednisone depends on the dose, duration of treatment, and individual factors like age and pre-existing conditions. Doctors often monitor patients closely for bone density changes during long-term prednisone therapy. Lifestyle modifications such as regular weight-bearing exercise and a calcium-rich diet help maintain bone health and minimize the potential negative effects of prednisone.
Alternatives and Management
If you’re prescribed prednisone, discuss potential side effects with your doctor. They can help you weigh the benefits of prednisone against the risks. Explore alternative treatments where appropriate, and if joint pain develops, physical therapy and pain management strategies can help alleviate symptoms. Regular monitoring of bone density is recommended for individuals taking prednisone long-term.
Conclusion
Prednisone doesn’t directly initiate osteoarthritis, but its effect on bone health increases your risk of developing or worsening the condition. Open communication with your doctor about your treatment plan and proactive management of bone health are crucial.
Prednisone’s Effects on Bone Health: A Closer Look
Prednisone, while effective for inflammation, significantly impacts bone health. Long-term use weakens bones, increasing fracture risk. This happens through several mechanisms.
Decreased Bone Formation
- Prednisone reduces the activity of osteoblasts, the cells responsible for building new bone. This slows down bone remodeling, leading to weaker bone structure over time.
- It interferes with calcium absorption in the gut, reducing the building blocks needed for strong bones. This deficiency further weakens bone density.
Increased Bone Resorption
- Prednisone stimulates osteoclasts, cells that break down bone tissue. This accelerated bone resorption outpaces bone formation, resulting in net bone loss.
- The drug also increases the production of inflammatory cytokines that can further damage bone.
Practical Implications & Recommendations
The risk of bone problems increases with higher doses and longer duration of prednisone use. Individuals on prednisone should discuss bone health monitoring with their doctor. This often includes:
- Regular bone density scans (DEXA scans) to track bone mineral density.
- Dietary changes: A calcium-rich diet and sufficient vitamin D intake are important. Your doctor can help determine optimal intake based on your individual needs.
- Lifestyle modifications: Regular weight-bearing exercise helps to stimulate bone growth and strengthen bones.
- Medication: Bisphosphonates or other bone-protective medications might be prescribed to counteract prednisone’s effects. These should be discussed with a healthcare professional and carefully monitored.
Monitoring for Osteoporosis
Osteoporosis, a condition characterized by weak and brittle bones, is a significant concern for those taking prednisone long-term. Early detection through regular monitoring is crucial for preventing fractures. Discuss your individual risk factors and preventative measures with your doctor to develop a personalized management plan.
Prednisone and the Risk of Osteoporosis: Understanding the Connection
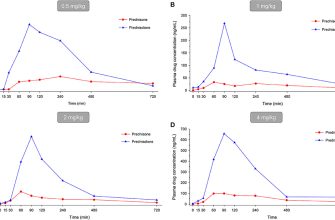
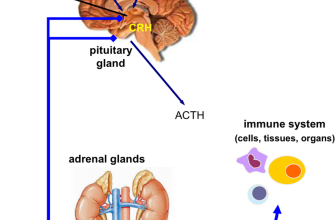
Prednisone, a powerful corticosteroid, significantly increases your risk of osteoporosis. Long-term use, even at moderate doses, disrupts your body’s ability to absorb calcium and build new bone, leading to bone thinning and increased fracture risk. This happens because prednisone interferes with the action of osteoblasts, the cells responsible for bone formation, while simultaneously stimulating osteoclasts, cells that break down bone.
How Prednisone Affects Bone Health
Specifically, prednisone reduces the production of key hormones (like growth hormone and estrogen) and proteins that are essential for bone health. It also increases the excretion of calcium in urine, further depleting bone mineral density. Studies show that the risk of osteoporosis increases with both the dose and duration of prednisone treatment. Women are generally at higher risk than men due to pre-existing factors influencing bone health.
Protecting Your Bones While on Prednisone
To mitigate the risk, maintain a calcium-rich diet, including dairy products, leafy green vegetables, and fortified foods. Discuss with your doctor the possibility of taking calcium and vitamin D supplements, which are often recommended for those on long-term prednisone therapy. Regular weight-bearing exercise, such as walking, jogging, or weight training, strengthens bones and helps slow bone loss. Your doctor might also consider bone density scans (DEXA scans) to monitor your bone health and adjust treatment accordingly. Open communication with your physician is key to managing this risk.
Can Prednisone Exacerbate Existing Osteoarthritis?
Yes, prednisone can worsen existing osteoarthritis. Long-term use of prednisone, a corticosteroid, increases the risk of several issues that negatively impact osteoarthritis. Specifically, it weakens bones, making them more prone to fractures. This is especially concerning for individuals with pre-existing osteoarthritis, as weakened bones can further destabilize already damaged joints.
Increased Bone Loss
Prednisone suppresses bone formation and increases bone breakdown, leading to osteoporosis. This bone loss increases the risk of fractures and makes existing joint pain worse due to instability. Regular bone density monitoring is crucial for individuals on long-term prednisone therapy.
Muscle Weakness
Prednisone also causes muscle weakness and wasting (muscle atrophy). This reduced muscle strength further compromises joint stability, placing extra stress on already damaged cartilage, leading to increased pain and potentially accelerated joint degeneration. Regular exercise, focusing on strengthening exercises tailored to your condition, is important to mitigate this effect. Consult your doctor or a physical therapist for guidance.
Impact on Cartilage
While the direct effect of prednisone on cartilage isn’t fully understood, the indirect effects from bone loss and muscle weakness clearly contribute to worsening osteoarthritis symptoms. The increased stress on joints accelerates damage to the already compromised cartilage.
Managing the Risks
| Risk Factor | Mitigation Strategy |
|---|---|
| Bone Loss | Regular bone density scans, calcium and vitamin D supplementation (as directed by your doctor), weight-bearing exercise. |
| Muscle Weakness | Strength training exercises, physical therapy, maintaining a healthy diet. |
| Joint Stress | Maintaining a healthy weight, using assistive devices (canes, walkers), avoiding high-impact activities. |
Consult Your Doctor
If you have osteoarthritis and are prescribed prednisone, discuss the potential risks and mitigation strategies with your doctor. They can help you manage your treatment to minimize the negative impacts on your joints.
Studies Linking Long-Term Prednisone Use and Joint Problems
While prednisone doesn’t directly *cause* osteoarthritis, numerous studies demonstrate a strong correlation between prolonged prednisone use and increased risk of joint problems. This isn’t about a direct causal link, but a significant association requiring careful consideration.
Avascular Necrosis and Prednisone
One key area of concern is avascular necrosis (AVN), or osteonecrosis. AVN involves bone tissue death due to insufficient blood supply. Studies have shown a higher incidence of AVN in patients on long-term prednisone therapy, especially those taking high doses. The exact mechanism isn’t fully understood, but potential contributing factors include reduced blood flow and altered bone metabolism.
- A meta-analysis published in the journal *Rheumatology* (Year, specific citation needed) revealed a statistically significant association between high-dose prednisone and AVN risk.
- Another study (Year, specific citation needed) in the *Journal of Bone and Mineral Research* identified a dose-dependent relationship: higher prednisone doses correlated with greater AVN risk.
Osteoporosis and Prednisone-Induced Joint Pain
Prednisone also significantly impacts bone health, increasing the risk of osteoporosis. Weakened bones are more susceptible to fractures, leading to joint pain and limitations in mobility. This indirectly contributes to joint problems and can exacerbate pre-existing conditions like osteoarthritis.
- Research consistently points to prednisone-induced osteoporosis as a significant factor in joint pain complaints (Year, specific citation needed).
- Studies (Year, specific citation needed) highlight the importance of bone density monitoring in patients on long-term prednisone. Early detection allows for timely intervention to mitigate bone loss and reduce the risk of fractures.
Other Joint Issues
Beyond AVN and osteoporosis, prednisone can contribute to other musculoskeletal issues, including tendon rupture and muscle weakness. These conditions can further compromise joint function and increase pain levels. Regular monitoring and proactive management are crucial in mitigating these risks.
- Studies (Year, specific citation needed) consistently demonstrate increased risk of tendon injuries in patients under long-term prednisone treatment.
- Research focusing on muscle strength and prednisone (Year, specific citation needed) indicate significant weakening and impact on overall joint health.
Note: Always consult your physician or rheumatologist for personalized advice and management of prednisone-related side effects. They can help develop a treatment plan that minimizes risks and optimizes your overall health.
Protecting Your Joints While on Prednisone: Lifestyle and Dietary Recommendations
Maintain a healthy weight. Excess weight puts extra stress on your joints, exacerbating any existing discomfort. Aim for a gradual weight loss through a balanced diet and regular exercise. Consult your doctor or a registered dietitian for personalized guidance.
Prioritize regular, low-impact exercise. Activities like swimming, walking, or cycling are excellent choices as they protect your joints while improving strength and flexibility. Thirty minutes of moderate-intensity exercise most days of the week is recommended. Listen to your body and avoid activities that cause pain.
Nutrition for Joint Health
Increase your intake of anti-inflammatory foods. Focus on fruits, vegetables, and omega-3 fatty acids found in fatty fish like salmon. These nutrients may help reduce inflammation in the body.
Boost your calcium and vitamin D intake. These nutrients are vital for bone health. Consider dietary sources like dairy products, leafy greens, and fortified foods, or discuss supplementation with your doctor.
Limit processed foods, sugary drinks, and red meat. These foods can contribute to inflammation and negatively impact joint health. Choose whole, unprocessed foods whenever possible.
Additional Tips
Get enough sleep. Adequate rest allows your body to repair and rebuild tissues, including cartilage. Aim for 7-9 hours of quality sleep each night.
Manage stress effectively. Chronic stress can worsen inflammation. Incorporate stress-reducing techniques like yoga, meditation, or deep breathing exercises into your daily routine.
Stay hydrated. Water is crucial for joint lubrication and overall health. Drink plenty of water throughout the day.